What is the likely future course of my PAH?
You likely had lots of questions about pulmonary arterial hypertension (PAH) after being diagnosed, such as “What is the life expectancy of someone with PAH?” and “How is PAH going to affect me?” So how do PAH specialists answer these questions about your unique PAH?
There’s good news: We have better answers to those questions than ever before. Our understanding of PAH and how to manage it have come a long way in recent years. Research has led PAH specialists to adopt an approach to better monitor and treat PAH. It’s called “risk assessment.”
Risk assessment allows your PAH specialist to predict your life expectancy when they determine what kind of treatment plan may be most appropriate for you.
Getting regular risk assessments and knowing your risk status could be the first step to feeling better and improving how you’ll do in the future (your “prognosis”).
Risk assessment provides a fuller picture of your unique PAH
Risk assessment is a way your healthcare provider can better understand your disease. It enables healthcare providers to see a fuller picture of your unique PAH by combining your individual test results into a single “risk status”—high, intermediate, or low risk.
Healthcare providers can then use your “risk status” to predict your chance of survival over the next 5 years and determine if your treatment plan is working.
Risk status helps determine your prognosis based on data from other patients
Risk assessment is an approach based on research and data from thousands of patients. Like you, these patients were all unique, but when PAH specialists looked at data from all of the patients together, clear patterns emerged. Those patterns identified the most meaningful tests your healthcare provider can perform, and how to combine the results to determine how you’re doing now and predict your prognosis for the future.
Risk assessment is new for many people, including some healthcare providers. A PAH specialist will be experienced in using risk assessment to predict PAH prognosis and guide your care. That’s why it’s important to find a PAH specialist.
What is risk assessment?
Dr. Lana Melendres-Groves explains risk assessment and why it’s so important.
So, what is risk assessment? This concept is at times very difficult to understand, even for me, who's been doing this for quite some time, but it's a different way of looking at PAH. We now know that this risk assessment is so essential to how we treat our patients that it's actually become part of our treatment guidelines. It's recommended that patients receive a risk assessment from their provider on their risk status at least every 3 to 6 months. This measures how well your treatment plan is working for you and it informs your healthcare provider if potentially changes should be made.
What does risk assessment reveal about my life expectancy?
Knowing your risk status helps you and your doctor estimate your life expectancy (specifically, your chance of survival over the next 5 years).
Your risk status is the result of a risk assessment, after your unique test results are combined. There are 3 main risk status levels: low, intermediate, and high risk.
For many patients and their specialists, the goal is to reach low-risk status because it is associated with better outcomes.
- your PAH treatment plan is working
- you may be walking farther
- you may have fewer symptoms
- you may have a better life expectancy over the next 5 years
- your PAH treatment plan may need adjustments
- you may not be able to walk as far
- you may have more symptoms
- you likely have a more moderate life expectancy over the next 5 years
- your PAH treatment plan should be adjusted urgently
- you may not be able to walk without getting breathless
- you may have more severe symptoms
- you will likely have a lower life expectancy over the next 5 years

Most people with PAH are at intermediate risk, even after starting an initial treatment plan. Treatment guidelines recommend patients and their specialist strongly consider making additional treatment plan adjustments if patients are not making progress getting to low-risk status within 3 to 6 months.
To help them decide how to make better recommendations to update their treatment plan after diagnosis, PAH specialists may split intermediate risk into 2 categories.
- Intermediate-low risk describes individuals at intermediate risk who are closer to low risk
- Intermediate-high risk describes individuals at intermediate risk who are closer to high risk
A specialist’s insight on life expectancy & risk status
What is the life expectancy of PAH patients? That is a question that I would say is very individual to each patient, each provider in terms of that discussion, so I don’t want to try to put specific time frames because I think that this is something that has evolved over the past 30 years. We can look back to our trials and registries that looked at life expectancy for patients with PAH back in the 1980s and early 90s, and we know that prior to the advent of specific medications for PAH patients, the prognosis with the diagnosis of PAH was very poor. Often, my patients will google or find online that they may have 2 to 5 years to survive after their diagnosis. I would say to that is that, over the course of the last 25 to 30 years, we’ve now been able to develop a multitude of therapies and best practices to be able to care for our patients. We can look back to one of the United States registries that was performed back in 2006 to 2009 timeframe, and we saw that we were already improving our patients’ outcomes with therapies, and that was over 15 years ago. And since then, multiple other therapies have been approved as well as our understanding of what we should be doing for our patients. So I think that the way that we look at life expectancy now is more individual to how somebody is doing, so every time a patient comes into my clinic, the goal is to try to understand where they are in their journey. That means looking at multiple tests, including blood tests and walk test and echocardiograms, and maybe even a new heart catheterization. And then, through a lot of that data, being able to assess where their risk status is. So I want to always come back to risk status, because I would say that knowing what someone’s risk status is to, you know, in some ways, helps us to predict how they may do long-term. Getting individuals to that low-risk status we know improves prognosis tremendously—that out at 5 years upwards in the 90% rang, people are surviving, Now, in situations where we may not be able to get somebody to low risk, then there may be other conversations that need to be had. But that would be the question that I would advise you to ask your providers; it’s “what is my risk status?” What does that mean in terms of my prognosis?
How is PAH severity (mild, moderate, or severe) different from risk status?
Healthcare providers sometimes use terms like mild, moderate, or severe PAH to describe how PAH affects an individual. These days, you may still hear these terms used informally, but they are not well defined and don’t reflect the best way to understand PAH disease status.
Risk status is another way to describe PAH severity, but the terms low, intermediate, and high risk are more clearly and consistently defined. Because of this, risk status is a much more useful way to understand PAH disease severity. Risk status describes the specific results of a risk assessment looking at your unique combination of test results.
Can risk status change?
Risk status doesn’t have to stay the same. In fact, it can get better or worse. Your treatment plan, lifestyle, and PAH progression can all impact your risk status.
If your risk status worsens, or if you haven’t improved to low-risk status, your healthcare provider may propose an adjustment to your treatment plan.
Learning more about the types of PAH treatments available can help you better understand your options.
Types of PAH TreatmentsRisk status: A closer look
In this video, Dr. Lana Melendres-Groves shows an example of how a risk assessment is completed.
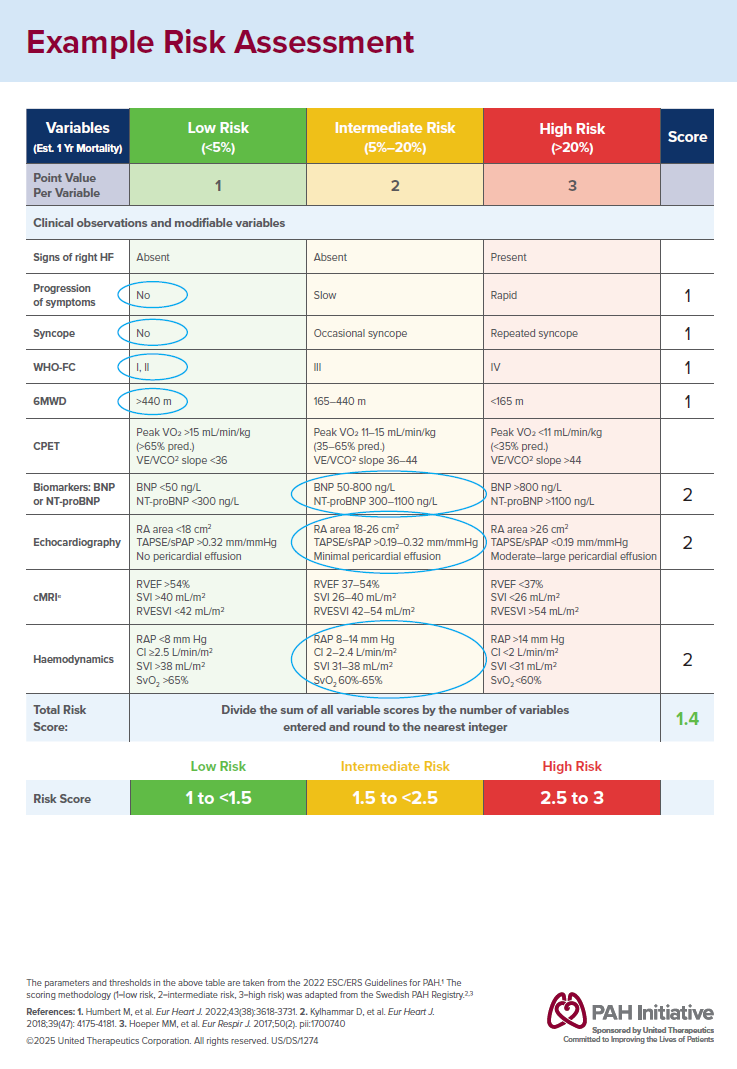
This is just an example of what a risk assessment looks like. It’s a table that often we color code in green, yellow, and red, because, you know, I think it helps us, just visually, to understand if we’re getting somebody to where they need to be. There’s a lot of information in this table, but we use all of those tests that we ask you to get to be able to fill it out. And it often looks something like this, where maybe you’re feeling quite good and are in a low-risk category, in the green category for how you feel and what you can do. But maybe some of the blood tests that we’ve gotten or some of the other procedures that you’ve done would indicate that actually you’re in more the yellow zone. We take all of those together and are able to come up with a score that indicates a risk status, and here, demonstrated in the bottom corner with 1.4. Knowing whether someone fits into a green zone, low risk, an intermediate zone, the yellow, which is intermediate risk, or in the red zone, high risk, we’re able to know if somebody will do better and have a better chance of survival over the next 5 years or if maybe there’s a lower chance of survival over that time frame.
What happens during a risk assessment?
During a risk assessment, your healthcare provider will perform many tests and evaluations. These tests and evaluations are the ones that were found in clinical trials to be the most meaningful in determining your current health status and how you’ll likely be doing in the future. These evaluations include the 3 listed below, as well as many others.
Your risk assessment includes:

6-minute walk test
During a risk assessment, your healthcare provider will measure how far you’re able to walk in 6 minutes. This 6-minute walk test gives clues about how your heart, lungs, and blood vessels are doing.

NT-proBNP/BNP
PAH can cause your heart to work harder than normal, which releases high levels of the hormone NT-proBNP/BNP. When this test shows high levels of NT-proBNP/BNP, it means your heart is working harder than normal.

Functional Class
Functional Class is a strong predictor of life expectancy, and it’s an important factor that your healthcare provider uses when choosing your PAH treatments. Functional Class evaluation consists of 4 categories based on the symptoms you experience when doing everyday activities.
The specific tests used in a risk assessment may differ. Learn more about PAH tests.
Download example risk assessment
You can take this sample risk assessment form to your next appointment to help guide your conversation with your healthcare provider about your risk status.
Example Risk Assessment PDFHow often should healthcare providers perform a risk assessment?
Because risk status can change, PAH treatment guidelines state that it’s important for healthcare providers to check PAH risk status when starting a PAH medication and at least once every 3 to 6 months after that. That way, healthcare providers can determine if their current treatment plan is working.
Not every test may be repeated as part of every risk assessment. Some tests may only be done periodically (not every visit), in which case your healthcare provider may use your most recent test result.
What types of treatments are available for PAH?
PAH treatment includes medications that help to restore balance among natural substances that help keep blood vessels healthy.
Types of PAH Treatments