Clinician resources
The PAH Initiative offers online resources and in-office tools, including patient education resources, to help you and your patients with pulmonary arterial hypertension (PAH).
Risk calculators
Quickly calculate your patient's risk status online.
At diagnosis
REVEAL 2.0
2022 ESC/ERS Treatment Guidelines
During follow-up
REVEAL Lite 2
COMPERA 2.0: 4‑Risk Strata
French Noninvasive Criteria
How to use calculator tools:
Download Instructions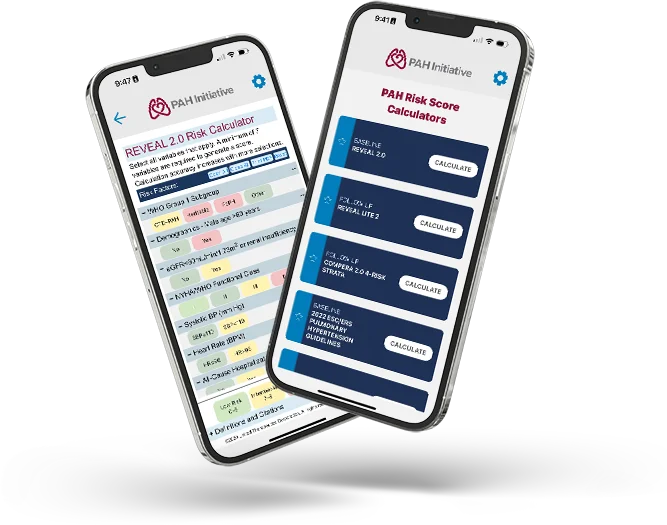
PAH Initiative Risk Score Calculator App
Examine the new Risk Score Calculator App that PAH Initiative created
Go to Risk Calculator AppIn-office tools and resources
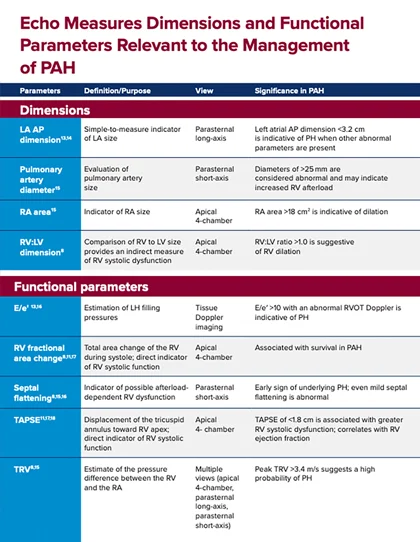
Right Heart Parameters
Use this guide to review key right heart parameters relevant to PAH management.
Right Heart Infographic
Use this infographic to review critical right heart assessments for PAH care.

Risk Calculation Worksheets
Use these REVEAL 2.0, REVEAL Lite 2, 2022 ESC/ERS Treatment Guidelines, and COMPERA 2.0 4-Risk Strata calculation sheets in your office as a quick reference when calculating risk.
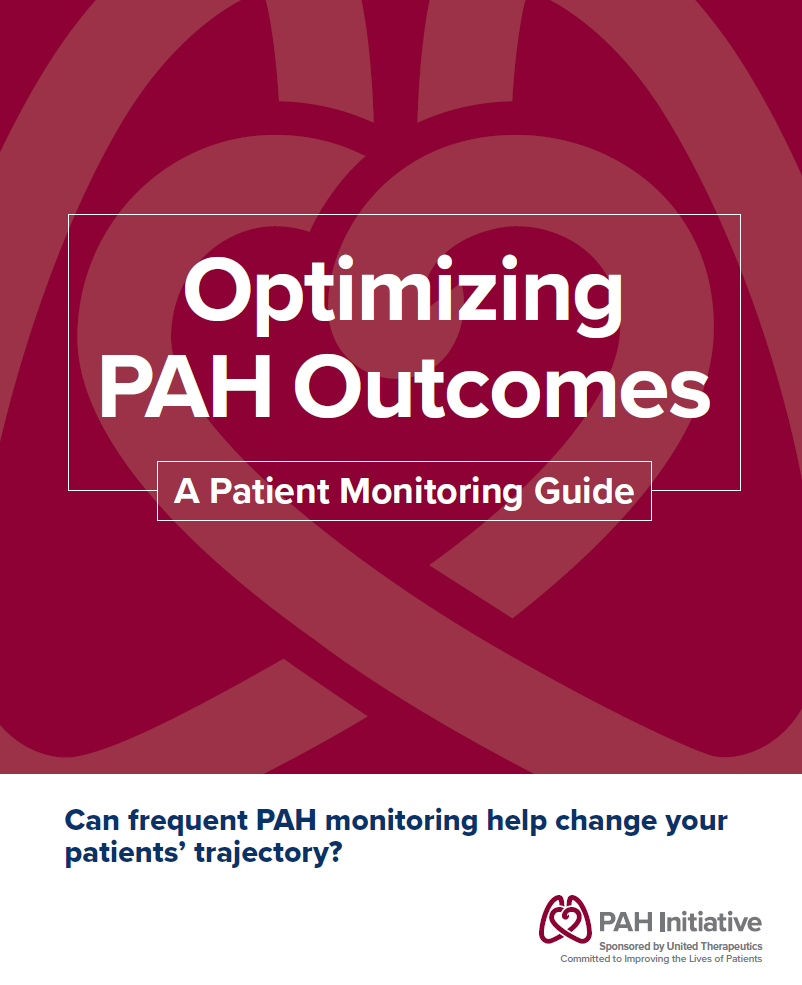
PAH Monitoring Guide
Review key elements of monitoring risk status and right heart parameters in your PAH patients.

Patient Intake Form
Use this form to better understand how your patients are feeling.

6-Minute Walk Test “How‑To” Guide
Use this guide to standardize how you measure your patient’s 6MWD.
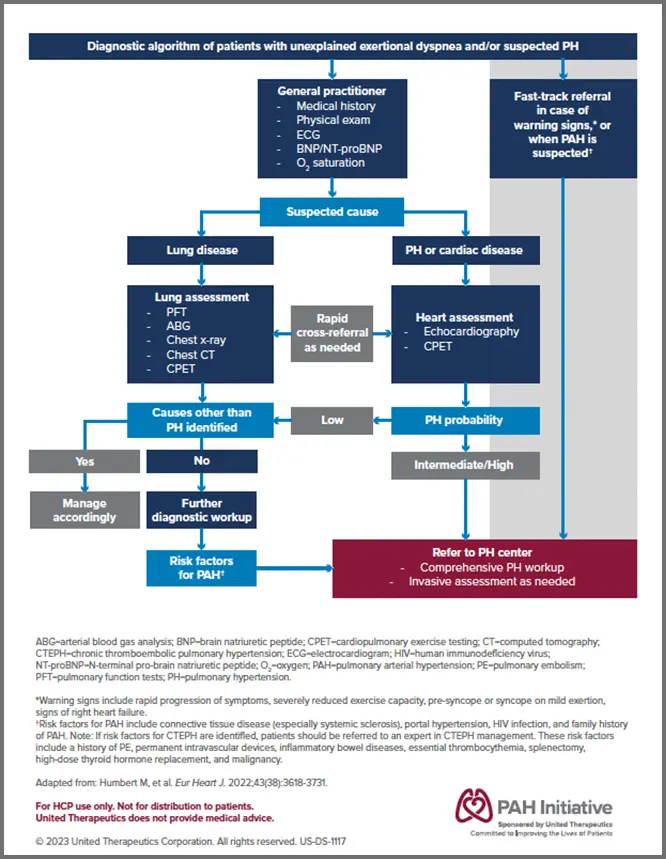
Diagnostic Algorithm
Use this diagnostic algorithm in your office as a quick reference when screening patients for PAH.

Publication List for the 2024 World Symposium on Pulmonary Hypertension
Quick access to download a list of key publications from the 2024 World Symposium.
Podcasts
Learn how experts stratify risk in their patients to improve prognosis by using objective, multiparameter risk calculation methods—and how applying this knowledge may help increase your patients’ chances of survival.

The Importance of Risk Assessment
Discover why formal risk calculations are essential and the latest tools available to you.
Dr. Raymond Benza: Welcome to the Pulmonary Arterial Hypertension Initiative podcast. This podcast is sponsored by and the presenters are being compensated by United Therapeutics. In this series of podcasts, we will talk about how PAH treatment guidelines and risk calculation drive treatment decisions in pulmonary arterial hypertension, as well as their own experience in treating our patients with PAH. My name is Dr. Raymond Benza.. And I have the pleasure of being with one of my longtime colleagues, Dr. Vallerie McLaughlin.
Dr. Vallerie McLaughlin: Hi Ray. It's great to be here. I'm looking forward to this podcast.
Dr. Raymond Benza: Thanks Val. In today's program, we will be discussing the importance of risk assessment and pulmonary arterial hypertension management. According to the PAH treatment guidelines, risk assessments should be driving our initial therapy choices as well as any changes in therapy. So let's get started. So Val, can you describe to me what risk assessment is all about in pulmonary arterial hypertension?
Dr. Vallerie McLaughlin: Yeah. Ray. I think that we as cardiologists have really incorporated risk assessment into really many different diseases. We use different scores for NSTEMIs and STEMIs, and CHADSVASC for AFib. We live this, this is really something that is important to objectively care for patients. And over the years, we have learned about the important parameters that are prognosticative in patients with pulmonary arterial hypertension. We've learned from many databases that have included thousands of patients, the parameters that assess a patient's risk or the severity of their illness and what their likelihood is of having an event over time. I think the multiparameter approach is really critical because this is a very complex disease and there are many different predictors, including how the patient is feeling, whether or not their right ventricle is failing, what their symptoms are like, syncope, how dyspneic they are, what their Functional Class is. Those are all clinical assessments of other patients. Echo has not been incorporated as much as I would like to see it.
We are really just more recently getting savvy about quantitating right ventricular function. I think we both know how that right ventricle function is really critical in terms of the outcomes of PAH patients. And then of course, hemodynamics are important. They define the disease and also reflect the function of the right ventricle. And so when we talk about a multiparameter risk assessment, we're looking at many of those different parameters and trying to assess whether we think our patient is at low, intermediate, or high risk over the ensuing years. And we learned from each registry that no matter what the treatment is, our goal for the patients to reassess their risk and to drive them into that low-risk status. Ray, is this your approach as well?
Dr. Raymond Benza: It is my approach. And I think you really eloquently described the available nuances that we take into consideration when we do these assessments of risk, including very importantly, the multiparameter approach. We never hang our hat on just one variable. And I also wanted to really emphasize the piece about imaging because, as we'll talk about it a little bit later, many of the contemporary tools that we have lack sophisticated imaging parameters as part of them. And I think the tools that we have and that we use and that we will describe later, have to be really used in conjunction with some of these other newer things that are coming out that we think are important, but achieving low risk and using the multiparameter approach, I think of the 2 salient issues that I really would like our practicing clinicians to take away from this.
Dr. Vallerie McLaughlin: Yeah. I agree. Let's talk about how often we should be performing those risk assessments. What's your approach to that?
Dr. Raymond Benza: I think at least at baseline is probably one of the most important parts of risk stratification. Really, when a patient comes to your clinic for the first time, they may not have been on therapy. They're just newly diagnosed. They're really assessing their baseline risk; it’s very, very important. Not only for the treatments that we decide to place them on, but also for the patient's information and their own means to plan their lives for the next year or 2. And then after that initial assessment, and I think at minimum, every 3 to 6 months, we should be evaluating our patients, but I'd like to get your opinion on a more detailed approach and maybe peaking at a patient every time we see him in our clinic. What do you think about doing risk assessments even in our routine clinic?
Dr. Vallerie McLaughlin: Oh, Ray. I think that's really key. I do that every single time I see a patient, I think pretty much every encounter we had and a patient, it's an opportunity to assess their risk and consider whether or not we've gotten them into that low-risk status because that's where we want them. So we can look forward and have confidence that they're going to do well. So Ray, there are lots of ways to assess risk. Maybe we should go on and talk about some of those methods and you were really the genius behind REVEAL risk calculators. Why don't I talk about the ERS approach, ESC approach, and the French approach. And you talk about REVEAL, if that's okay with you?
Dr. Raymond Benza: That's perfect Val.
Dr. Vallerie McLaughlin: Yeah. The ESC and ERS guidelines published this table, the very famous table. Green, yellow, red stoplight sort of table about a number of different prognosticators in pulmonary arterial hypertension and cut points that put them at low, intermediate, or high risk. Most of these are derived from registry data. Some of them are derived from gestalt, right? Like syncope is really a gestalt thing and an observation that we've made, but not really included in registries. So the important determinants include Functional Class. So we know patients who have Functional Class 4 symptoms do very, very poorly and Functional Class 1 and 2 do well, and Functional Class 3 sort of in the middle. We have discussed hall walk already, the exercise tolerance, objective exercise tolerance is something that's very important and that can tell us about a patient's prognosis. So greater than that sort of magic 440 number of patients do well, less than the mid-100 patients do poorly.
The Echo data and well, this is different; something I actually would like to talk to you about. The Echo data in all of these is really very limited. The presence of a pericardial effusion, which has been published a few times and the size of the right atrium—that's really the data that we have from registries that go into these scores. When I do an Echo on a patient, I go look at that right ventricle. It really is very meaningful to me and, I think, anyone who has experience in this disease. I think that it's unfortunate that many registries don't have a quantification of right ventricular function. Not all Echo labs quantify right ventricular function. I just thought maybe you'd want to comment on that, Ray, before we move on.
Dr. Raymond Benza: Oh no, I agree with you 100%, Val. I think all the tools that we have developed were developed in eras when imaging wasn't as prominent as a known risk player in prognosticating. And I agree with you that as these risk scores and equations evolve, that I would love to see more imaging data in the scoring systems. And I think the important thing about that is if you really look at the spectrum on how a patient evolves or progressed this with PAH, we have changes in pressure that then lead to changes in the right ventricle. And these changes can occur very early, even before many of the other symptoms or variables that are accounted for. So it even might add a level of greater sophistication and predictability for early decompensation by including these imaging parameters, entities, contemporary scoring systems that we have.
But ultimately, I think that it's the combination of these things that are important, as you mentioned earlier, the ESC and ERS guidelines and even the French method, which use a number of variables that are within the guidelines. There are some differences between the calculators that we have developed in the REVEAL, but I was curious if you might want to go into a little bit more about some of the French methodology for calculating risks before I went into what we do with REVEAL.
Dr. Vallerie McLaughlin: Yeah, for sure. In fact, let me just make a couple more comments on ERS, ESC. So we talked about the syncope, right ventricular failure, Functional Class, hall walk or cardiopulmonary exercise testing PCO2 is listed. Biomarkers are also included BNP less than 50, NT-proBNP less than 300. Very good prognostic indicators puts the patient in a low risk. Whereas if the BNP is greater than 300 or NT-proBNP is greater than 1400, that puts the patient in a higher risk. And then of course, hemodynamics are also important in terms of risk. And we've known for many years, and this point is emphasized in the risk assessments. It's not what the pulmonary artery pressure is. It is how the right ventricle is coping with that pulmonary artery pressure. So, right atrial pressure, cardiac index, and SPO2 are the hemodynamic parameters that are most predictive. So, that's the ERS, ESC approach.
Now the French approach, which I really like, is very simple. They took a different approach. They basically said, these are the 4 factors that are most important to us. And it has to do with being in Functional Class 1 or 2, having a hall walk over 440, having a cardiac index greater than 2.5, and a right atrial pressure less than 8. And so those are the 4 factors using the invasive French approach that they look at. And if you have 3 or 4 of those 4 factors, your prognosis is very good. Whereas if you have less than that, the prognosis is quite poor.
And then when they had a subgroup of patients that also had biomarkers and they can incorporate the BNP or NT-proBNP, when you put that into the multivariate analysis, the right atrial pressure and cardiac index falls off. And so the noninvasive French is really just Functional Class, hall walk, and biomarkers. And at least for me, that's something I do in clinic every time I see a patient. I have all 3 of those parameters every time I see a patient. So that's the noninvasive French approach. Ray, you want to tell us about REVEAL?
Dr. Raymond Benza: Yeah. Thanks Val. So REVEAL calculators are in essence, very similar to the ESC/ERS guidelines and the French method in that they both use very similar variables. And that's good because that tells us that all the contemporary restratification scoring and systems that we use are complimentary. And we could feel safe using them because many of the variables are shared. REVEAL takes it just a little bit further down kind of the statistical pathway, than the guideline or French method in that REVEAL methodologies are really derived from very standardized statistical modeling. And very importantly, that the variables that are used in these scoring systems are weighted against each other so that the relative importance of one variable versus another. For example, the Functional Class may be more or less important than an NT-proBNP level. So it kind of gives you a way to really summate the risk with a little bit more sophistication than some of the European methods.
So REVEAL Lite 2 is the derivation of an earlier model called REVEAL 1.0, and what REVEAL 2.0 did is, it took a lot of the same variables that we had found in the original REVEAL 1.0 calculator. Which contains both demographic vital signs and other more objective measurements and add it to that hospitalization and the risk that is imparted by recent hospitalization for pulmonary hypertension and heart failure. It gave us some more objective means of measuring renal function, which we know comorbidities are very important part of risk stratification and renal function is one of the very important ones that have been highlighted and uses a GFR and then set of a subjective assessment of renal insufficiency. And also changes some of the scoring points and actually add a more of a dynamic nature to the changeable risk factors like BNP and the 6-minute hall tests.
So it takes those variables and then weights them And you can calculate a score that very nicely discriminates between low, intermediate, and high risk. Now, the difference between REVEAL 2.0 and REVEAL 2.0 Lite is just the number of variables that's required to make the calculation. The parent score, which is the REVEAL 2.0, scores 13 variables that are associated with it. And these contain some immutable risk factors. The factors that don't change over time, like a patient type of pulmonary hypertension that they have and their gender and age, even though age does change the risk points, here it is a kind of a combination of age and gender. And then it has a number of easy-to-discern variables, including vital signs like low blood pressure or high heart rate combined with the Functional Class NT-proBNP levels in which there are several cut points and 6-minute walk distance, which also has several cut points.
And then add that the Functional Class and Echo estimates of pericardial effusion that you mentioned earlier, and then hemodynamics, which include importantly, the right atrial pressure and the pulmonary vascular resistance. And then REVEAL Lite, take the parent calculator and really strip it down to the easily obtainable, changeable variables that you can assimilate in each clinical encounter. Very similar to the French method and that it uses vital signs, Functional Class, the hall walk test, the NT-proBNP levels, and the vital sign. But the big differences, as we mentioned earlier, is that these factors continue to be weighted against each other, such that the discrimination index with these more statistically derived methods are a little bit higher than those that don't incorporate weighting. Well, I hope those descriptions of the algorithm and calculators were helpful to the audience, but I'd like to ask Dr. McLaughlin, if she has any further opinions or statements that you wanted to make about the formal risks calculations that we make?
Dr. Vallerie McLaughlin: I think that was a really elegant discussion of how REVEAL was developed. And one thing I want to highlight is the difference between 2.0 and 2.0 Lite, including the nonmodifiable risk factors. I think when we have nonmodifiable risk factors in a risk calculator is an excellent way to predict prognosis. In fact, I think there's probably nothing more accurate at actually predicting prognosis than REVEAL 2.0. But sometimes when we think of driving people to low risk, we get a little challenged because there are so many nonmodifiable risk factors in it that, sometimes our patients are going to be at very high risk, no matter what we do. And that I think is one of the things that we've discussed over the years about using calculators and driving patients to the low-risk status. And I think REVEAL 2.0 Lite very nicely addresses that issue and really includes the risk factors that you can treat with medical therapies and have success at trying to drive patients into a low-risk status.
I think that's a really important differentiation and in fact, REVEAL 2.0 Lite and French are very similar with the exception of the additional parameters of vital signs and kidney function. I think we've discussed 4 different tools and they're all very good. They're all very meaningful. If you get into low-risk status with any of those tools on therapy, no matter what the therapy is, the patient's prognosis is good and that's what we're looking for to improve the patient outcomes. And so that leads us to the next discussion point. We have this really wonderful data from all of these risk calculators that show if we can get them to low risk, they do well. So let's talk a little bit about why it's so important to use a formal risk calculator rather than just the gestalt. Do you have any comments on that, Ray?
Dr. Raymond Benza: Yeah. Thank you Val, for pointing that out. I think that is really important. And as we mentioned earlier in the talk, these tools are very complimentary to each other, and I think that can be used together a more formalized, detailed risk assessment would REVEAL 2.0 perhaps at baseline and maybe at a year. And then when you're doing the peak of patient, like you mentioned earlier, watching them at each one of their clinical visits, maybe that's the time where you can implement the French method or REVEAL Lite. To get those on the fly risk assessments, just so that you make sure that you are actually plotting the trajectory correctly. Clinical gestalt, they think can really mislead us in certain circumstances. Now we even have a recent study that compared clinical gestalt and the form of risk calculation, and by reviewing patient's charts from clinicians who treat patients with PAH. And both clinical gestalt and the calculated risk were aligned in less than half of the 365 charts that they examine.
I've found that very surprising 80% of the patients that are estimated to be low risk by clinical gestalt were actually reassigned to a higher risk category and perform a risk calculation. That's really important because underestimating risk is where patients can really be hurt because that's where you would use as an intensive mode of therapy, as opposed if they were really low risks. So that's a really important thing is just not to miss the intermediate or high-risk patients by utilizing a less nuanced way of predicting risk. And I think there have been other studies that looked at formal risk calculation in these earlier patients functional two class patients.
And I believe a retrospective chart analysis of 153 Functional Class 2 patients who were either on mono- or dual combination therapy. And more than half of the Functional 2 patients were classified as intermediate or high risk when the risk was calculated. So again, these are patients whom if we use the single variable of assessment like Functional Class or even clinical gestalt, we would have underestimated their risks and perhaps not put them on the intensity of therapy that the patients deserve to be on.
Dr. Vallerie McLaughlin: I think those are great points, Ray, and I think we always have to have some common sense, some gestalt in medicine, but this is an example where risk calculators are helpful. But I might point out Functional Class, as we've talked about, is subjective. Maybe a patient sounds Functional Class 2 because they've limited their activities so much that they don't get short of breath. A really skilled historian can try to dig that out, but sometimes patients just adapt in it. It's also leads to the next topic of discussion is relying too much on one thing such as Functional Class. I mean, for many years before we had all of these additional tools and all of the additional data about BNP and what have you, Functional Class was the holy grail and it's something that's easy. It's inexpensive, we do it every single time we see a patient. But it's not enough, is it?
Dr. Raymond Benza: No, it's not. And it's like you said, we uproot the weed on Functional Classes, cardiology fellows. And it's been ingrained into the way that we evaluate our heart failure patients, but it is the bottom-line subjective. It really relies on patient input, their memory, and even their honesty at some point. And so this objective evaluation really has to be weighted and thought of in a different manner. The formal risk assessment is objective. We're talking about multiple parameters. Some that are objectively measured, but not subjectively measured like human dynamics or vital signs or pericardial effusion on an echo or an NT-proBNP level. So, balancing these subjective with objective factors I think is very good, but I don't want to short come the Functional Class because even despite its subjective nature and every risk calculator and every assessment we have done, it's always peaked its head is something that is important. It may not be as discriminatory as the others, but it certainly remains important.
Dr. Vallerie McLaughlin: Yeah, no question. Now, some people who are critics of this say, "Oh my gosh, it takes so much time. You have a limited amount of time with a patient appointment and epic or the electronic medical record makes it all so complex. I don't have the time to do this over the course of a visit." And I think that's really not a very good excuse to do something that is so important and so prognostic for a patient. A French invasive or noninvasive is really for 3 variables. It really doesn't take that much time. And Ray, I know that you've actually gone to a lot of trouble trying to develop apps to make the REVEAL calculation easy as well.
Dr. Raymond Benza: Yeah. So, there are apps that are currently available. There are websites that are available that can calculate the risk for you. We've made a lot of headway in some of the EMR and programming them to calculate risks on the fly. So I think the nature of the calculation is getting easier and easier for practitioners to perform. But like you mentioned, doing a risk calculation using REVEAL Lite 2, or the French method that can be done in less than 30 seconds. So it really is very, very easy to do and my practice, my nurse coordinators calculate the risk before I even walk into the room. And so it's readily available for me to talk with the patient about and discuss and make critical decisions on.
Dr. Vallerie McLaughlin: Yeah. Ray, I think you've contributed so much to this area. It's really been a delight to have this conversation with you. I think to wrap up, we've really emphasized that formal risk calculations are important to help us monitor our patients and choose the appropriate therapy for them. So it's been such a pleasure and this concludes our first PAH initiative podcast. Please join us next time when we will discuss initial therapy choices based on risk calculation.

Initial Therapy Choices and Treatment Goals
Learn how our hosts determine initial therapy for their patients.
Dr. Vallerie McLaughlin: Hello, and welcome to this PAH Initiative podcast. This podcast is sponsored by and the presenters are being compensated by United Therapeutics. In this series of podcasts, we will talk about how PAH treatment guidelines and risk calculation drive treatment decisions in PAH, as well as our own experiences in treating our patients with PAH. I'm Dr. Vallerie McLaughlin
Dr. Raymond Benza: And I'm Dr. Raymond Benza. It's a real pleasure to be here with my close colleague, Dr. McLaughlin.
Dr. Vallerie McLaughlin: Ray, it's always a pleasure to work with you. I really enjoyed our first podcast during which we discussed the importance of risk assessment in PAH management. In this program, the second in our series of podcasts, we're going to discuss initial therapy choices based on risk assessment. So let's get started with that. Ray, let's say you've just met a patient, you've just diagnosed a patient with PAH, how do you determine their initial treatment plan? There's so many things to consider and so many agents that are now available to treat PAH. What's your approach?
Dr. Raymond Benza: Well, I agree with you. I think that's one of the nice things about treating pulmonary arterial hypertension in this era is that we do have so many available agents to treat this disease. As you know, when we both trained, there was only 1 therapy for this disease, and now we have at least 12 to choose from. So, understanding how to use these medicines intelligently to both make patients feel better, function better, I think is really important. And I think the common ways that we do that now, as we talked about in our first podcast is to really use a multidimensional approach that evaluates a person's summated risk, and then base our treatment therapies on that summated risk, whether you use the REVEAL calculator or one of the European systems, this multidimensional risk paradigm is really very important.
And I think the guidelines say that most patients who are judged low or intermediate risk should receive upfront oral combination therapy, and that those who are at high risk conversely, should really receive combination therapy that includes an IV prostacyclin-class therapy. And then again, as we mentioned in our first podcast, our treatment goal is really to get patients to low risk and then monitor them continuously. And again, always reassessing, always trying to drive them to this low-risk goal, because we know that that improves not only mortality for these patients, but also makes it a much less morbid disease. they're functioning better in their own home environments.
Dr. Vallerie McLaughlin: Yeah, I think that was a great summary, Ray. So I agree. In my practice, probably a very small proportion, maybe less than 10% of patients are at such high risk would we make the diagnosis that they go onto parenteral prostacyclin therapy as part of their combination therapy. The vast majority of patients are intermediate risk and there are some low risk. And we use upfront combination therapy generally with an ERA and PDE5 to start out with in most of our patients. What's your practice, Ray?
Dr. Raymond Benza: I agree with you. I think we need to be very careful in this category. One, because we know that PAH is a progressive disease, and we want to make sure that we halt this disease in its track. And just the combination of several medications really seems to do a good job trying to really slow down the disease. But as you mentioned, there are few people who can be started on monotherapy. And I believe these are the people who are extremely low risk. For example, having 4 of the low-risk factors by the European methods or REVEAL score less than or equal to 5. These people usually have a low risk, both of morbidity and mortality, and may be an ideal patient to use monotherapy on. But again, I want to caution everyone that when you use these multimodality risk factor parameters, as we mentioned in our first podcast, you should use these together both with your clinical gestalt and with other modalities that are not defined in these contemporary restratification systems, particularly imaging of the right ventricle.
So if I see someone who's low risk, but their right ventricle is still not looking good, that's not a patient for monotherapy. These are people who usually have really well preserved, right ventricular function. They're low risk by these contemporary scores, which includes a low Functional Class, a low pulmonary vascular resistance, a low mean pulmonary artery pressure, and as I mentioned and stressed, a normal right ventricle at Echo. And we have had people who've been treated with monotherapy for more than 5 to 10 years on a long-term basis and are stable with a low-risk profile. But the key is here, you have to continually reassess to make sure that these patients that you're treating with a singular drug really stay low risk in the long term. So again, constant reassessment, as we talked about in the first podcast is really, really very important. And then obviously, as you mentioned, Val, when combination therapy is either unavailable or contraindicated, because a patient may have severe liver disease as an example, that you get may be an indication for that. Therefore, monotherapy is really the exception and not the rule.
Dr. Vallerie McLaughlin: Yeah. I think that was a really wonderful summary, Ray. I just want to focus a minute on those low-risk patients. We're still recommending combination therapy on low- and intermediate-risk patients with the exception of some of these patients with extraordinarily low-risk status that you described. Those patients, at least in my practice, are few and far between. Ray, what's your experience?
Dr. Raymond Benza: Oh, no, I agree with you. And that's why I really want to issue this word of caution to be really careful that you really scrutinize this low risk to the highest extent that you can, because you don't want to do these patients a disservice. Just was going to agree with you, Val that my experience actually, very, very few patients are in this very low-risk status as you mentioned. So caution, I think is the key word here.
Dr. Vallerie McLaughlin: Yeah. I would say the patient population that I tend to see in that very low-risk status at the time of diagnosis are those patients who are very aggressively screened in our scleroderma clinic and they get diagnosed with PAH with a mean pulmonary artery pressure in the low 20s and a pulmonary vascular resistance of just barely over 3, with a normal right ventricle. Don't see them that often, but that's the group that I tend to see them in. But let's say, Ray, you diagnose a patient, you start them on a treatment plan. We have really emphasized the goal of getting them to a low-risk status. How do you monitor them? What's your approach to reassessing them for that risk status? And how do you approach the continued management after that first initial treatment decision?
Dr. Raymond Benza: Well, as we mentioned, Val, and you and I had this really great discourse in that first podcast, that really achieving the low-risk status is our goal. And this is supported by multiple registries looking at thousands of patients. And we know that people who achieve low-risk status live longer, function better than those who remain at intermediate or high risk. So that's something that's always got to be in the background when you're evaluating these patients on a continual basis. And that again is the really key piece here. These are patients that you just can't see, start them on a medication or walk away with them. They need to be constantly reevaluated, constantly restratified. And as we mentioned in our first podcast, using very simple algorithms like the European low-risk criteria or REVEAL Lite 2, which has very simple to garner modifiable factors, we can really restratify them every time we see them in clinic, or even over the telephone in some instances, to make sure that their trajectory is following the path that we want them to.
But certainly we want to officially see these patients after starting them on new therapy, certainly within 3 to 4 months to do a good risk assessment, probably using an imaging modality in addition to the contemporary restratification systems that we do. Some people, if they're moving really aggressively in the wrong direction, could add another set of hemodynamics to that, again to reassess the patient in totality, to make sure that we're pushing them into low-risk status. And if we're not, then we need to intensify therapy to really get them moving in the right direction.
Dr. Vallerie McLaughlin: Yeah, I agree with that, Ray, and I just want to emphasize one point, and that is the timeline. I would have to say that my practice has evolved to be a little bit more on the aggressive side. We do a nurse practitioner virtual visit at 1 month just to make sure they're tolerating the therapies well. We find that that helps with retention on therapy. We can talk them through some side effects, and I'm now really leaning toward that 3-month time point to bring them back into the office and reassess their risk and decide if we need to escalate therapy. So I think that is really important, as you've emphasized, get them to low risk.
And I think it's 3 months for... I think 6 is stretching it, but let's move on to aligning goals. We're physicians, we have studied this, we have this vision of improving long-term outcomes of our patients. And we know with all the data that you have reviewed that getting them into the low-risk status improves their outcomes, but really what the patients want is to feel better, right? They come to us, [inaudible 00:11:38] they come to us not being able to go up the stairs. What they want is to feel better. They want to feel less short of breath. They don't want to have a lot of side-effect medications. We really need to align our treatment goals with the patient's lifestyle goals and their goals for their everyday day-to-day living. Can you tell me a little bit, Ray, about how you incorporate that in your practice?
Dr. Raymond Benza: Yeah, Val, I think of the many things that we've talked about today, this is one of the most important aspects of therapy that is often neglected. Patients have to be involved in your decision making at every point. Physicians at times, get too focused on mortality and morbidity and really what the patient wants is, as you mentioned, they want to feel better. They want to breathe easier. So incorporating the symptoms in your treatment paradigms are really important. And we use simple tools like the emphasis questionnaire, or even sometimes even more complex questionnaires to really get a good idea how the patient's really in functioning and feeling in their own environment. And we use these quality-of-life measures in determining how aggressive we need to be. Is there a balance between side effects of medications when they're on combination therapy where they're not really feeling well because of side effects? So you really have to take the balance of how a patient feels from a quality-life-perspective and the intensity and aggressiveness of your medical management.
Dr. Vallerie McLaughlin: Yeah, I think that was well said, Ray, and I think it's really critical to involve the patients. I did a video visit earlier today on a 19-year-old gentleman with heritable disease. He's not where we want. And probably one of my most important questions to him is, “Tell me what you want to do that you can't do right now” and setting those goals, trying to figure out what it is the patients want in their lifestyle and how to balance that with the side effects of the drug. So, it's really critical. And I would also want to emphasize that this is a tremendous opportunity to involve the rest of our allied healthcare professionals. Many of these medications have side effects that are complex to manage, and sometimes patients give a little more information to nurses and nurse practitioners than they do to physicians. And I feel very fortunate and I suspect you are as well, Ray, to have such a wonderful team of nurses and nurse practitioners who really are partners in managing this disease, particularly when it comes to the lifestyle issues of the patients.
Dr. Raymond Benza: Yeah, Val, thanks for bringing up that very important point. I really love the idea of patients articulating their goals at the beginning of therapy and the incorporation of all the wonderful allied health professionals, as you mentioned, into this decision tree so a patient really feels taken care of as a total person. It is really important in setting the trends for their long-term therapies.
Dr. Vallerie McLaughlin: Well, Ray, it's always a pleasure to chat with you. I enjoyed our podcast today on this very important topic of therapy choices and risk assessment. I'd like to thank the audience for joining us today for these discussions as well. Join us the next time to discuss monitoring patients over time and considerations in escalating therapy for patients who are not at low risk.

Therapy Escalation
Learn how to clinically apply risk status to determine when to escalate therapy and help improve patient prognosis.
Dr. Raymond Benza: Welcome to the PAH Initiative Podcast. This podcast is sponsored by, and the presenters are being compensated by, United Therapeutics. In this series of podcasts, we will talk about how PAH treatment guidelines and risk calculation drive treatment decisions in PAH, as well as our own experience in treating our patients with PAH. I'm Dr. Raymond Benza. And I have the pleasure today to be interchanging with a very good friend of mine, Dr. Vallerie McLaughlin.
Dr. Vallerie McLaughlin: Hi, Ray. Thank you for having me. It's great to be here.
Dr. Raymond Benza: In our last podcast, we discussed initial therapy choices in PAH and the importance of risk assessment in those decisions. In today's program, the third in our series of podcasts, we will discuss the need for regular risk assessments in PAH and escalating therapy, in order to help our patients achieve the low-risk status. So let's get started.
And Val, we know that our risk calculation needs to be performed to determine a patient's initial therapy regimen. After your patient begins their initial therapy, when are you performing risk calculations to assess whether they're meeting their treatment goals? And does this change based on the type of patient that you're looking at?
Dr. Vallerie McLaughlin: Yeah, Ray, that's a really important question. I think we have spent a lot of time over the years focusing on what's the right initial treatment, and obviously that's a very important question. But I think what's even the more important question is, where do we get with that initial treatment? What is that patient's risk? And do we need to do more?
I'll tell you, patients often ask me when they're diagnosed, "What's my prognosis? How long do I have to live?" And I tell you, I don't even want to answer that question at the time of diagnosis anymore because what's more important than what the risk status is at the time of diagnosis, is where they get in terms of their risk status on therapy.
So, that initial treatment choice is important, but it needs to be followed up. We need to reassess them on therapy to see if they're meeting the criteria for the low-risk status.
We tend to reassess our patients within about 3 months. We may call them over the phone before that 3-month visit, to make sure they're tolerating their therapy, and they're sticking with it, and that their side effects are well controlled.
But we'll generally bring pretty much all of our patients back to clinic within 3 months and reassess their risk, at the very least the assessment of Functional Class, the physical exam, the hall walk, biomarkers, often imaging as well. And we'll do an objective risk score, as we've talked about.
There are many from which to choose. REVEAL, which you've been so instrumentally involved in, Ray, the French, either invasive or noninvasive, or the ERS/ESC approach, but you need to do some objective assessment and determine whether or not the patient's at low-risk status. And if they're not at low-risk status, then you need to escalate therapy. And there are obviously many choices to do that.
Dr. Raymond Benza: Yeah, I think you brought up some very important points. The initial diagnosis and risk stratification really sets the tenor of that initial therapy, but it's really the follow-up assessment that really tells you what that trajectory is going to be and if that patient's moving in the right direction with that initial therapy.
So, I agree that second assessment is so important and having that done at least by the 3-month mark, after you're starting a therapy, I think is a really appropriate way to do it. So thanks for highlighting that.
So, when you see a patient and currently they're still at intermediate risk, how long would you wait before escalating their therapy?
Dr. Vallerie McLaughlin: Well, Ray, I think that's an important question. I would do it at that 3-month point. I don't think that waiting much longer is really going to benefit the patient. And, in fact, it may harm the patient.
I think the key there is intermediate risk. Intermediate risk, to me, is such a wide range. I hate to get too technical but, in my mind, there's low intermediate. There's high intermediate. I look at these patients in very different ways, and I know you do too. And the REVEAL risk score kind of delineates this a lot as well.
So, I definitely think at 3 months, if we are still in intermediate risk, we need to do something else. But then there's the opportunity to tease things out a little bit more, to determine how that should be done.
Dr. Raymond Benza: Yeah, I think that's a really important point, to really know where they fit in that intermediate range, because it is really a very big gray area for us. But I agree with you 100%. Don't leave people in intermediate risk. That's really important.
Why is it so important to be proactive in assessing patients and adding therapies when needed? And I know we talked a little bit that the last question, but given the progressive nature of the disease, are patients at risk for disease progression, even when symptoms are absent?
Dr. Vallerie McLaughlin: Well, Ray, PAH is a progressive disease. It's a disease with a high risk of mortality, even in patients who are on therapy. It is not uncommon that our patients sort of start compensating for themselves and adjust to a new way of life. In fact, there was a recent retrospective chart analysis that looked at 153 Functional Class 2 patients. And remember Functional Class 2 is just one of the parameters that we look at, but these are patients who are basically saying they're okay. But when you do objective assessments on them, a very high proportion of them are really technically at intermediate risk, or some even at high risk.
There's also that one paper that I love to cite. I think it's from the Amsterdam group, that does serial walks and MRIs and clinical assessments. And you'll look and see at their patients, the ones who deteriorate, and you will see changes in their MRI before they start telling you their symptoms are worsening.
So, I think we need to, again, rely on the multiparameter assessment, and we really need objective data to try to assess these patients' risk.
Dr. Raymond Benza: Yeah, that's a great point. If you think of this disease as a continuum, really, symptoms are really late manifestation of progression. So things could be going on, cellular changes, changes in hemodynamics and resistance, and even subtle decompensation of the right heart, that may not be felt at the time that it's happening, really trying to put together this multimodality approach, even in the asymptomatic patients, is really, really important to make sure they are truly at low risk, not only for mortality, but for morbidity too. Because remember, a lot of the scoring systems that we use are really focused on mortality, but you want to get into systems that also give you that risk of morbidity. And you want your patients to be at low risk, both for mortality and morbidity. So that's really important when you make the assessments, like you mentioned.
Dr. Vallerie McLaughlin: Yeah, I think, Ray, it's really important to mention that, if you wait too long, sometimes you never catch up. Dr. Raymond Benza: Exactly.
Dr. Vallerie McLaughlin: Right? We've seen this in clinical trials. We've seen this with placebo groups in clinical trials, that when therapy is delayed, they just don't improve as much as the patients who got active therapy early on. We've seen this in meta-analysis that patients, if you let their 6-minute walk deteriorate too much, they never catch up.
And, so, I think that is a really great argument for us to be more proactive about those treatment goals and about the timing of those assessments and getting to those goals.
Dr. Raymond Benza: Routine and regular monitoring is really the thought for the day, I guess, when we really think about it. When would you decide to actually prescribe a prostacyclin-class therapy?
Dr. Vallerie McLaughlin: Ray, I think that's a great question. And, again, you and I, we can admit, we're a little older. We grew up with parenteral prostacyclins. We're very comfortable with prostacyclins. And if they are not at low risk at their reassessment, it's time to consider a prostacyclin pathway agent.
Certainly, if a patient has high-risk symptoms and criteria, objective criteria, not meeting the French low-risk criteria, high REVEAL score, they're at high risk. And we often move to a parenteral prostacyclin therapy on them. Even some of the patients who are kind of at the high end of intermediate risk.
I think we have to keep our mind open to them and keep our patients' minds open to them, if they're in that higher-risk status.
However, if the patient is at intermediate risk, maybe they're a little better, but they're not meeting low-risk criteria, we have many other options, including different oral prostacyclin pathway agents, as well as inhaled.
Dr. Raymond Benza: Yeah, that's a really good point. I guess this is where really good communication between practitioners is really paramount. For those who you mentioned who have a little hesitation because they haven't had a lot of familiarity with this class, communication with an experienced center, to kind of help that practitioner through this with their patients is really, really key in the management schemata, so that patients really get the right drugs at the right time.
Dr. Vallerie McLaughlin: And this goes back to the excellent point you made about communication, Ray. We have to have open communication with our patients as well, and our nurses who tend to know the patients well, to determine their treatment goals, assess their risk, to think about how aggressive we need to get, and balance that with the side effects of the therapies.
Dr. Raymond Benza: Yeah, I think it's really important to message, as we both mentioned, that practitioners shouldn't be afraid to use prostacyclins in patients at a higher risk status. And if you don't know how to use it, just reach out for help, and there's always someone there.
When we use prostacyclins, what would you typically expect to see when you add this agent to a patient's regimen? What are the benefits that you might see from that?
Dr. Vallerie McLaughlin: Well, that's an excellent point, and it's something that needs to be emphasized with the patient, as we have goals with these agents. We've been talking in this series about risk, and it would be obvious to say we're trying to improve their risk profile. But the patient doesn't really care about the risk profile at that moment. They really care about how they feel.
So, there's data on prostacyclin-class therapies, about improving symptoms, improving Functional Class, improving hall walk, improving hemodynamics. These therapies improve a patient's ability to function, as they set their goal, whether that goal is to be able to take care of their kids or get back to some recreational exercise or be able to go up the stairs and do their job without shortness of breath.
They delay disease progression. And that's one of the reasons why we try to use them in patients who haven't achieved their risk.
These, of course, have to be balanced with the side effects. We know this class of agents have a number of side effects, including headache, diarrhea, jaw pain, nausea, sometimes musculoskeletal symptoms, flushing. And, so, we need to make sure the patients understand that, and that they understand the risks associated with the delivery system. Septicemia, bacteremia, if they're on IV. Cough in inhaled. Sometimes the GI side effects are worse on the orals.
So we need to make sure the patients understand that and understand that we will work with them and have lots of tricks up our sleeve to monitor those side effects and help obviate them.
But the whole reason that we're doing this is to improve their symptoms, improve their functional capacity, and improve their outcomes.
So you see what I just did there, Ray? I call that the benefits sandwich. You tell the patient why you're going to use that therapy, what to expect on the upside, our goals in terms of improving their symptoms and getting them back to what they want, have them set some goals.
Be careful. You have to tell patients about the side effects. We don't want to blindside them. So we go through the side effects and reassure them that we will be there to help them manage the side effects, but then put the other slice of bread on the sandwich. Remember, the whole reason we're doing this is so that they feel better, that they're able to do the things that they want.
Dr. Raymond Benza: Yeah. Val, what you just said really resonates with me. The goal for patients can be very different than the goal for physicians, and they really should align. A patient's conception of risk, they may not really be able to fully appreciate what that means for them while they're still having active symptoms.
So it's really important really to drive those symptoms to a state where a patient can really accept the importance of reducing their risk.
So, I really liked that sandwich approach, and I'm actually going to use that terminology the next time I see a new patient, is talk about the therapy sandwich. I like that.
Well, Val, thank you so much for joining me today for our discussion on timely treatment escalation. And I thank the audience for their listening in. And please join us next time, when we discuss the difficult conversations that we have with our patients regarding disease progression and management.

Conversations With Your Patients
Discover which topics are the most important to bring up with your patients during their PAH treatment.
Dr. Vallerie McLaughlin: Hello, and welcome to the PAH Initiative podcast. This podcast is sponsored by, and the presenters are being compensated by, United Therapeutics. In this series of podcasts, we'll talk about how PAH treatment guidelines and risk calculation drive treatment decisions in PAH, as well as our own experiences in treating our patients with PAH. I'm Dr. Vallerie McLaughlin. And I'm joined today by my good friend and colleague Dr. Ray Benza. Ray?
Dr. Ray Benza: Good day, everyone. Val, it's a pleasure to be here speaking with you again on this very important topic.
Dr. Vallerie McLaughlin: Yeah. Thanks, Ray. It's always a pleasure. As you know, in our previous podcast, we discussed the importance of frequent risk assessment and timely treatment escalation. We talked about that from our physician and PH treater viewpoint. But today, we would like to discuss the conversations that we have with our patients who have PAH, including the discussions around risk assessment, treatment, escalation, and their prognosis.
Let's talk about those conversations that we have with our patients. We see them, we assess their symptoms, we talk to them about their therapies, and we risk assess them. That really drives our monitoring and our treatment of our patients. So Ray, tell me how you talk to your patients about their risk status and why low risk is such a critical treatment goal and how we get there.
Dr. Ray Benza: Yeah, thanks for asking that, Val. I think that's probably one of the most crucial things that we do with our patient engagements in clinic. It's really important for them to understand the strength of restratification and how it really drives our methods of management for their disease. Usually, what I try to do is I try to have them understand how all the tests that they do come together to really develop a firm prognosis on how they do with their disease. So all these tests that they get, their walk tests, their functional class assessments, their blood work, their echo, their pulmonary function studies, and even their hemodynamics, how they all fit together into one unifying picture. And they paint that prognosis to their physicians who then gauge their therapies on them. So I typically will show them some of the tools that we use to assess their risk.
In our clinic, we typically use the REVEAL calculator. I show them how we plug in all the information that we've gathered about them into that calculator and how it spits out a specific risk of their one-year survival and morbidity associated with that disease. Sometimes, patients are even interested in seeing what their survival curves look like and how as they move from one score to another, how that prognosis can either become more poor or even improve as their therapy changes the course of their disease.
Dr. Vallerie McLaughlin: Yeah, I think that's great, Ray. One important component of any of these tools is functional class. Now, as we talk to a patient about their functional class, there is some subjectivity to that. Can you tell me how you assess a functional class on your patient during a visit?
Dr. Ray Benza: Yeah. This is really interesting, and I think it's such an intuitive question because we usually have a pattern of asking what limitations the patient has in their daily lives. And they always wonder why we ask them all those questions until you show them how it comes together that you develop this functional class assessment, which is an integral part of all these assessment tools that we talked about earlier on some of our podcasts.
Typically, I will usually ask a patient, "Are you short of breath when you're speaking to me?" which assesses really how a patient breathes at rest. If they're watching television, are they short of breath? If you're sitting at the table reading a book, are you short of breath? And then I will ask them increasing levels of exercise to really get an idea where their breathlessness starts. For example, do you get short of breath showering or shaving or putting your makeup on or doing your hair or dressing? Activities that represent daily activities of living. I'll then ask them, "Can you walk a block? Can you walk a flight of stairs?"
With each progressive increase, an activity where they develop breathlessness, I correlate that with their functional class, so that if they're short of breath at rest, they are functional class IV. If they're short of breath doing their daily activities of living, they are functional class III. If they're short of breath walking a block or a flight of stairs but okay at rest and with their daily activities of living, that's a functional class II. If they have no shortness of breath with any of their activities, that's a functional class I.
Dr. Vallerie McLaughlin: That's interesting, Ray. I mean, that just shows you the subjectivity. I approach it in a way that's very similar to you, starting with a low-level exertion and gradually going up, but I have different cut points than you do. A block or a flight of stairs, if they get short of breath with that, I'll call them a III. I would expect for most patients, that's an ordinary activity that they should do. It's really the second flight of stairs that I would call them a II. But I think the key is as long as you're doing it consistently within your practice, that's tells you the difference from one visit to another.
I think the other important thing with functional class is, really, what does the patient do? I think we all have some couch potatoes in our practice or some people who have just limited themselves so much that they'll tell you they don't get short of breath with anything, but they really don't do much besides walk around their house. How do you really sort of tease that out when the patients have a very limited activity level from the start?
Dr. Ray Benza: Yeah, I think these are where some objective measurements become very useful. We've developed surveys that patients can take while they're in the waiting room, which describe a whole level of different activities that they can check off to see whether they have shortness of breath or not. That way, you really keep that it's the patient's opinion, but you judge based on these various levels of activities what they can and cannot do and can maybe judge from that their functional class.
And there were other ways to do it. I agree with you. There are a number of patients who really sit around and don't do much activity during the day. That's where other tools may come in to be very helpful. Whether they use activity monitors or things like that, that give us an idea of how much functional activity they do per day and if they are really sedentary. And sometimes a more functional assessment is necessary to really get at their level of breathlessness.
Dr. Vallerie McLaughlin: Yeah. I think those are great points, Ray. You mentioned earlier that you discuss prognosis and you show survival curves to patients. Can you explain to me how you described that to patients and what their response is? I think that we all have challenges talking about issues like that. We want to bring hope to the patient. We want to talk in a positive way, but sometimes those curves are very enlightening. Tell me how you approach that and what the patients’ responses are.
Dr. Ray Benza: These are the nice things to have some sort of technology in the room with you. We do a lot of these discussions using our iPads, and we use animation on these curves so that we can say, "This is where you are right now, and this is what we would expect you to survive if we did nothing to you. But this is where we want to get you."
Then I keep showing them the animated improved scores and curves associated with those. And I say, "This is what we can do as we add therapies and if you respond to them." And that does give them a lot of hope that, "Wow, I can really improve my score. I can improve my prognosis" And I think that really brings them into really understanding their disease state and why we push so hard to achieve the low-risk status, because that's where we show them we want to get them. So, "Here's your curve. Here's where we want to get you. And we can do it by using thoughtful medications and additions, having you watch your exercise tolerance and report it to us accurately" and those types of things. I think that really gets them engaged in the conversation.
Dr. Vallerie McLaughlin: Yeah, I think that's really a great point. You know, so often we treat patients and they feel better. They think about their short-term goals. And now they're able to function better, maybe even their functional class and their hall walk have improved, but maybe they're still not really at low risk, but honestly they're happy with how they've improved in their quality of life. And sometimes, these conversations are the most difficult. The patient thinks they're doing fine and maybe they are in the short term, but we need to really explain the long-term goals to them. Tell me how you approach that conversation, both in terms of risk assessment and explaining long-term goals, but then also making that confident recommendation to them about an incremental therapy.
Dr. Ray Benza: Yeah. Wow, that is a really, again, another insightful question. I think that's how I kind of move the conversation is by talking about survival. And as you mentioned, maybe survival is not something that a patient is most interested in. They're more interested in quality of life. And so then I try to move the conversation from survival to morbidity, including hospitalizations or the risk of hospitalizations for heart failure or pulmonary hypertension related to heart failure. I think most patients would agree that they don't want to be hospitalized. And that would negatively impact on their quality of life, so that when you show them that there is an association between their risk level and the risk of them being hospitalized, well, that brings a few more patients into the equation.
Dr. Vallerie McLaughlin: Yeah. I think those are great points, Ray. And I think we also have to remember the shared decision-making paradigm, but how valuable as well our insight is for the patient, right? We are always balancing risks and benefits. And as we talk to patients about some of these more advanced therapies, if they're not at low-risk status, we need to weigh all of that. We need to talk about the potential benefits in terms of long-term outcomes, improving symptoms. We have to be honest with them about the potential side effects of these medications and the tools that we have to manage those side effects. But then, we really need to stress the fact that we are recommending this because we think it's in their best interests long-term, that we think it's going to improve their symptoms, quality of life, morbidity, and really make that confident recommendation to them. They rely very heavily on us for that.
Dr. Ray Benza: I agree. And I really think all the questions that you asked were so insightful today. I guess I would like to thank everyone in the audience for joining us today as we reviewed how we talk to our patients about different topics in pulmonary arterial hypertension. I would also ask them to be on the lookout for more podcasts where we will discuss important topics in the PAH space.
Dr. Vallerie McLaughlin: Great. Thanks, Ray. A pleasure working with you as always.
Dr. Ray Benza: Same here, Val.
If you would like more information on risk assessment, PAH treatment guidelines, or to use an online risk calculator, please visit pahinitiative.com/hcp.

PAH FC II: What’s Their Risk?
Learn the importance of formal risk calculation—even in FC II patients.
Dr. Raymond Benza: Welcome to the PAH Initiative podcast. In this podcast, we will be examining the importance of formal risk calculation in patients with Functional Class 2 pulmonary arterial hypertension. This podcast is a disease education program sponsored by, and the presenters are being compensated by United Therapeutics. No product information will be discussed in this podcast. Good day. My name is Dr. Raymond Benza. I'm happy to have today as my guest, Dr. Sandeep Sahay. Dr. Sahay, thanks so much for being here and I'm going to have you do the honor of introducing yourself.
Dr. Sandeep Sahay: Thank you, Dr. Benza and I'm so excited to be here with you. I am Dr. Sandeep Sahay. I'm a pulmonologist at Houston Methodist Lung Center, Houston Methodist Hospital, Houston, Texas. And my clinical work is primarily focused on patients with pulmonary hypertension and other pulmonary vascular diseases. I'm actively involved in clinical trials and clinical studies. I have my personal interest in portopulmonary hypertension, and I am trying to look for the genetic basis of this disease. I'm excited here to be with Dr. Benza and I will be discussing one of our recent publications about the physician gestalt and risk stratification.
Dr. Raymond Benza: Well, thanks very much. Dr. Sahay was the lead author on an important study, as he just mentioned, a risk assessment in patients with Functional 2 pulmonary arterial hypertension. This study evaluated physician gestalt and formal risk calculation in Functional Class 2 patients and assessed the factors that could explain any discordance between the two. This article can be downloaded at pahinitiative.com. Dr. Sahay and I are excited to share the study with you, so why don't we get started? So Sandeep, first question for you, according to the treatment guidelines, risk assessment is critical in the management of all our patients with PAH, driving both our initial choices and continued treatment escalation. Tell us a little bit about the conceptualization of this study with Functional 2 patients.
Dr. Sandeep Sahay: Thanks Dr. Benza. This question is actually a very important question because when we treat and manage patients with pulmonary arterial hypertension, there is a general perception among the clinicians taking care of these patients that Functional Class 2 patients are sort of doing well, they are stable. And, I think this study very much questions that stability. which is exactly what we highlighted in this study, that even though these patients are Functional Class 2, they can be in intermediate to high risk and at a somewhat higher level for disease progression and subsequently at higher risk for mortality as well.
Dr. Sandeep Sahay: What we showed in this study, that as per our perception, the patients who are thought to be in Functional Class 2, they were actually at much more higher risk by showing that when we applied the risk stratification scores, they were intermediate to higher risk or a high-risk category.
Dr. Raymond Benza: Oh, that's really interesting. We've used Functional Class for so long and I've often come to question its subjective nature. And so, formal risk assessment really takes a lot of that subjectivity out of the equation when you use that. And in essence, it really compliments and makes the single-set appointment of Functional Class much more comprehensive, I think. Well, let's examine this study design. Dr. Sahay, can you describe the physicians who participated in this study?
Dr. Sandeep Sahay: So, we included a variety of physicians and also, a variety of settings. So we had physicians who are pulmonologists and cardiologists. We included 38 pulmonologists and cardiologists in the United States. They did have a pretty good experience in managing PH patients on a median of like 60 patients per a year. And they were from diverse settings. There were many from academic settings, they were from a private tertiary level and PH comprehensive care centers. And we did analyze 153 patient charts for this analysis. As far as their baseline therapies were concerned, just keep it in mind that in this study we included only Functional Class 2 patients; 38% of patients were receiving monotherapy and 62% of patients were on combination with PDE5 and endothelin receptor antagonist combination. We did exclude the patients who were on prostacyclin-class therapy actively, or within the last three months. We did acknowledge some study limitations in our paper that obviously we were limited by the physician participation and the patient chart review. So we had a relatively small sample size for this study.
Dr. Raymond Benza: Thanks for that great summary. So in this study, we looked at physician gestalt and formal risk calculations. How were these obtained?
Dr. Sandeep Sahay: For physician gestalt, physicians were interviewed, and they were asked to provide their own risk assessment for each patient using their best clinical judgment. However, we aren't sure if physicians were using any sort of a risk stratification. To do the formal risk calculation, we used three different risk calculation methods, modified noninvasive version of French, COMPERA, and REVEAL 2.0, which included 13 parameters, including renal insufficiency and recent hospitalization. Again, the study limitations were because of the missing data. It was a retrospective study. We were not able to obtain all the parameters needed for each patient to calculate those risks.
Dr. Raymond Benza: Okay, thanks for that. Well, let's get to the results of the study. When risk was formally calculated, more than half of the Functional 2 patients in this study was shown to be intermediate or high risk. For example, using the French noninvasive method, 79% of the Functional 2 patients were classified as intermediate or high risk. Is this consistent with what you see in your practice?
Dr. Sandeep Sahay: Yes. This was a very exciting observation. And I think this finding is very much consistent. And as I recently started using in the last year, we have been using REVEAL 2.0 in our clinical practice. And I also noticed that almost 30 to 40% of my patients who I assumed, or I would say in my physician gestalt as low risk or doing well were actually not low risk. So, I'm very much convinced with this finding that this is likely true.
Dr. Raymond Benza: Yeah. We've seen something very similar in my practice and amongst my partners, that Functional Class tends to underestimate the comprehensive risk of a patient by about 30 to 40%. That's pretty interesting. Well, let's go on. When we looked at the congruence between clinical gestalt and formal risk calculation in these Functional 2 patients, it ranged from 43 to 54%, depending on the tool used. If we look at the patients assumed to be low risk by gestalt, 64% of these were reassigned to a worse risk category after formal calculation using the French noninvasive method. Among these patients considered to be low risk by gestalt, 4 to 28% were categorized as high risk using formal risk calculation. That's really amazing. What are the implications of under assessing risk on these patients' lives and long-term prognosis?
Dr. Sandeep Sahay: Well, I think one of the most important implications of this finding is if we are underestimating the risk for disease progression, that means we are undertreating our patients. As a result, we are increasing their risk for poor outcomes. Not achieving a low-risk status means you are heading for a worse prognosis.
Dr. Raymond Benza: Very interesting. So underestimating risk leads to undertreatment of patients. We're going to dig into that a little bit later in this conversation, but let's go on a little bit more here. What do you think the reasons for this incongruence was, based on your analysis?
Dr. Sandeep Sahay: This was one of the very interesting findings we observed in this analysis that, the physicians who were doing echocardiography less frequently were more incongruent with the risk stratification or formal risk assessment. I think one of the bases for this observation is that the echocardiography can pick up the progression or the changes much earlier than when the patients can report those symptoms to their physicians or changes in their Functional Class or changes in their six-minute walk distance. So, I think this was a very important observation of this study, that if you do echocardiography more frequently, you are less incongruent with the formal risk stratification-based risk assessment of your patient.
Dr. Sandeep Sahay: And I think this highlights another important factor that you should not just be looking at Functional Class to assess the risk. So, it's a very comprehensive multiparametric assessment for these patients. And, another important factor here is that physician-reported patient activity level. Patients with moderate or high activity levels are more likely to have incongruent risk assessment. And also physician-reported patient symptomatic stability and improvement over time. A patient may change the activities they perform to activities that are easier for them to accomplish, thus leading to a potential misassessment of Functional Class.
Dr. Raymond Benza: That's really interesting, and that's why formal risk assessment is really so important. And I think these data underscore the importance of frequent echocardiograms and risk assessment. How frequently are you performing Echos on your patients with PAH and does it differ based on the patient's status?
Dr. Sandeep Sahay: Depending on where they fall or what is going on, if I'm changing therapies, titrating prostacyclin, and all those factors play a role. But if someone who is on for routine follow-up, generally in our clinic, we follow them around three to four months. And at the same time, we do a full reassessment of their risk status with all the testing, which does include echocardiography. But at times, if you have a sicker patient, it's much sooner. Sometimes you have a very low-risk patient, we may prolong that to up to six months also. But generally, I would say most of the patients fall between three- to six- months period.
Dr. Raymond Benza: Yeah. That's a really important point that you brought up that echocardiography is so sensitive in that these changes in heart structure and function really precede the changes that we see in Functional Class, or even things like our six-minute walk test, like you said. Thanks for that information. Well, what do you think these results say about how we should be monitoring and treating our patients with PAH?
Dr. Sandeep Sahay: Oh, in these results, clearly one thing is highlighted that we should be performing a comprehensive risk assessment at each evaluation. Certainly, more frequent echocardiography showed more congruencies with the risk assessment, formal risk assessment of your patients. So, clearly our findings showed that formal risk assessment for the PH patient should be done or must be done at each interval when we reassess our patients.
Dr. Raymond Benza: So, Functional Class seems to underestimate risk when using formal risk stratification and symptoms are one of the last signs of disease progression. So we need to be really proactive in how we are monitoring and treating our patients with formal risk calculations and doing them every six months and according with the treatment guidelines. And again, stability is not good enough for Functional Class 2 patients; we really should be treating to low-risk status. And if you wait for these symptoms to worsen, you're already behind. Those are all great points. What would you like for PH-treating physicians to take away from this study?
Dr. Sandeep Sahay: So there are a few things I would like to highlight from the study. The number one is, like you mentioned that, I think Functional Class 2 is not the only way to really assess the risk of your patient. A comprehensive risk assessment with a formal risk calculation score is very much important and recommended by the guidelines as well. So please do not shortchange their chance to improve. And according to the guidelines like ESC/ERS guidelines that even at the time of diagnosis, and also at follow-up, we should perform a formal risk assessment. We should not just focus on the Functional Class as the determinant for their risk. Patients at intermediate or high risk should be considered for treatment escalation, including those at Functional Class 2. And watch for your own potential biases, when evaluating Functional Class 2 patients. Patients perceived as having symptomatic stability or higher activity levels can throw off gestalt-based assessment of risk.
Dr. Sandeep Sahay: More frequent Echos may help you identify risk change status more consistently, maybe a little bit earlier than the clinical presentation from patients. Overall, these results highlight the importance of formal risk assessment for all patients, particularly when they are Functional Class 2 versus a physician-based gestalt assessment.
Dr. Raymond Benza: Those points really resonate with me, Sandeep. And one of the things that I really like what you said was don't shortchange your patient's chance to improve. I think that's a really important sentiment that treating physicians should take out of this discussion that we're having today, that comprehensive and formalized risk assessment really takes the inconsistency out of the Functional Class as itself as a symptom of disease severity. And that we should be using formalized risk assessment as another tool in our tool belt that really compliments our clinical gestalt. So, this has been a really great discussion. I thank you for joining us today as we reviewed the importance of formalized risk calculations. And I thank my guest host Dr. Sandeep Sahay, for this very important article and these very important points for our treating physicians.
Dr. Sandeep Sahay: Thank you, Dr. Benza. I'm glad to participate in that. And I hope this podcast will help our listeners learn more about risk stratification and the gestalt-based assessment. Thank you. Thanks, everyone.
If you would like more information on risk assessment, PAH treatment guidelines, or to use an online risk calculator, please visit pahinitiative.com/hcp.
