PAH diagnostic criteria
Diagnosing pulmonary arterial hypertension (PAH) involves a series of tests, starting with an initial evaluation of symptoms, lab work, and imaging to assess heart and lung function. This process concludes with right heart catheterization (cath), the definitive step to confirm PAH by measuring pulmonary pressures directly from the right heart.1
Symptom onset
Symptoms are related to right ventricular dysfunction2
Typical presentation includes exertional symptoms2
- Dyspnea
- Fatigue
Due to nonspecific symptoms, the time between symptom onset and diagnosis is often >2 years3
Diagnosis
As disease progresses, symptoms start to occur at rest as the RV fails to compensate against the increased PVR2,4
- Syncope
- Lower extremity edema
- Abdominal distention
- Angina
Misdiagnoses/Comorbid conditions
Common misdiagnoses or comorbid conditions that delay diagnosis5,6:
- PH-LHD
- COPD
- Asthma
- Obesity
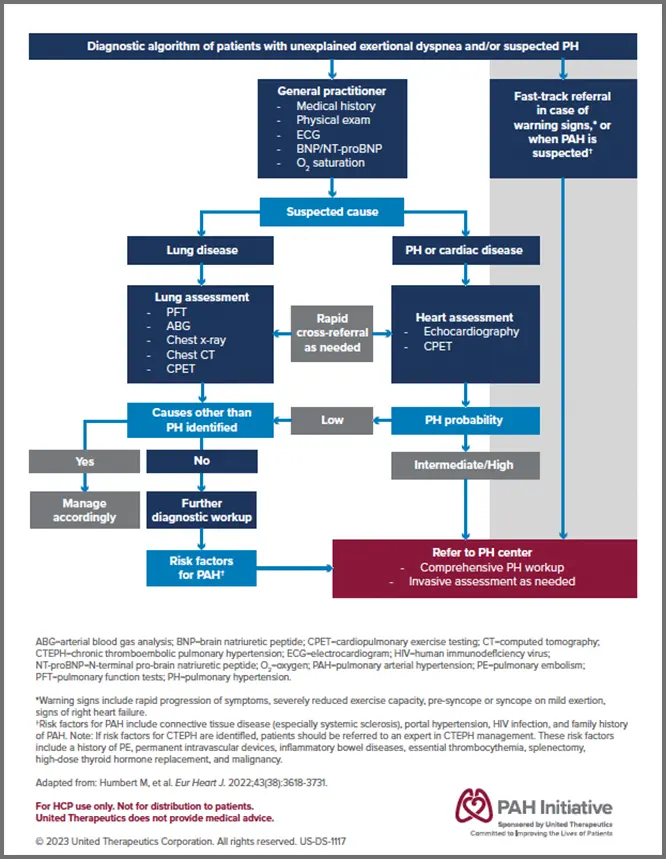
Diagnostic algorithm
The diagnostic process begins after clinical suspicion of PH based on symptoms and physical examination.1
Although many tests can hone suspicion of PAH, a right heart cath must be performed to definitively diagnose PAH. Current treatment guidelines recommend that patients be evaluated at a PH Expert Center for confirmation.1,2
Download a step-by-step guide of testing and decision-making to help reach a possible diagnosis of PAH.
Symptoms of PAH are often nonspecific7
Patients with PAH often present with nonspecific symptoms resulting from the decompensation of the RV. The delay in symptom presentation and the nonspecific symptoms of PAH lead to delay in diagnosis.3,7,8
Early symptoms2,6,9
-
1Dizzness
-
2SOB (dyspnea)
-
3Palpitations
-
4Fatigue
-
5Edema

Late symptoms6,8,9
-
6Syncope
-
7Jugular venous distension
-
8SOB
-
9Chest pain
-
10Hepatomegaly
-
11Swollen abdomen
-
12Low blood pressure
Screening for PAH1
Cardiac
- EKG
- Echo
- Cardiac MRI
Respiratory
- Pulmonary function test
- Arterial blood gases
- Overnight oximetry
Blood
- Laboratory tests (eg, blood counts, electrolytes, kidney function, uric acid, liver parameters, iron, BNP/NT-proBNP, thyroid testing)
- Immunology tests (anti-nuclear antibodies, anti-centromere antibodies, and anti-Ro)
- Serologic testing (hepatitis, HIV)
Exercise
- CPET
Imaging
- Chest radiograph
- V/Q lung scan
- Non-contrast and contrast-enhanced CT
- CTPA
- Abdominal ultrasound
Exam findings that may indicate PAH

Extracardiac exam findings4
- Jugular vein distension
- Hepatomegaly
- Peripheral edema
- Ascites
- Lung examination is usually normal
Cardiac findings reflecting functional and structural changes of the right ventricle4,10
- Left parasternal shift
- Loud pulmonary component of the second heart sound
- Pansystolic murmur of tricuspid regurgitation
- Diastolic murmur of pulmonary insufficiency
- RV third heart sound
Echo measurements may suggest PAH
A right heart Echo can assess the probability of pulmonary hypertension based on peak tricuspid regurgitant velocity and presence of other suggestive signs of the disease. However, right heart cath is required to confirm the diagnosis.1
Echo evaluation to hone PAH probability11
One way to investigate the probability of PAH based on Echo findings is to use VEST scoring. The VEST score uses routine variables from an Echo report to help determine the probability that a patient may have PAH.
Scores range from -3 to +3. If your patient has 1 “yes,” there is a probability that they may have PAH, and the more "yes" results, the higher the probability.
Patients with more "yes" results should be referred to PH Expert Centers for more comprehensive diagnostic investigations, including right heart cath.
Echo images may suggest PAH
These Echos show the progressive dilation of the RV and RA in PAH.
In end-stage PAH, the RV may cause the interventricular septum to bow outward and compress the LV.
Other signs of RV dysfunction that can be found on Echo include1,12,13:
- Tricuspid regurgitation
- Ratio between RV and LV basal diameter >1
- Loss of IVC inspiratory collapse
- TAPSE
- Increased RV systolic dysfunction
- Presence of pericardial effusion
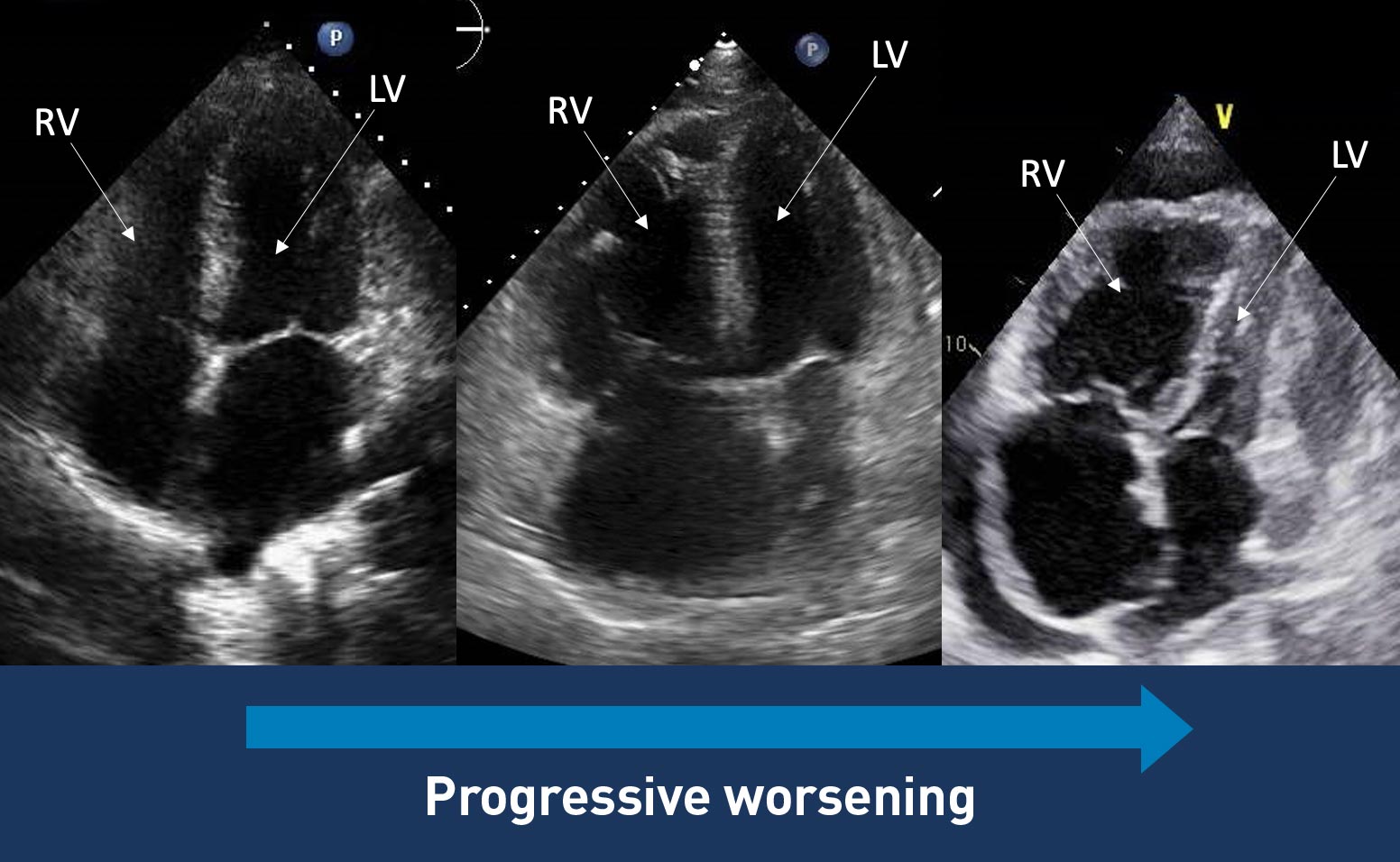 Images courtesy of Anjali Vaidya, MD, FACC, FASE, FACP. Pulmonary
Hypertension, Right Heart Failure & CTEPH Program, Temple University
Hospital.
Images courtesy of Anjali Vaidya, MD, FACC, FASE, FACP. Pulmonary
Hypertension, Right Heart Failure & CTEPH Program, Temple University
Hospital.
Explore the 2025 ASE Guidelines for Echo assessment of the right heart
Access 2025 ASE GuidelinesRight heart cath is required for a definitive diagnosis1
The 2022 ESC/ERS Treatment Guidelines recommend that patients with unexplained exertional dyspnea, syncope, and/or signs of RV dysfunction should be assessed for suspected PH/PAH using transthoracic echocardiography with a confirmed diagnosis ultimately dependent on hemodynamic results obtained from right heart cath.1
Hemodynamic values obtained during right heart cath1,14
- Confirm diagnosis of PAH
- Evaluate severity of PAH
- Assess congenital heart defects
- Exclude left-side heart disease
- Assess response to vasodilator challenge
- Assess key hemodynamic parameters
- Guide treatment decisions
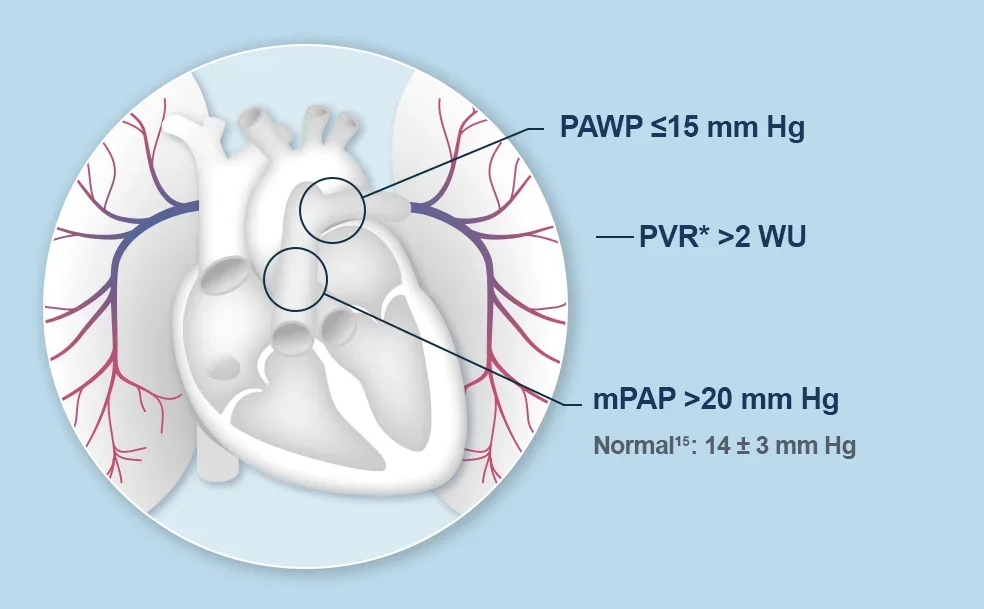 *PVR = (mPAP – PAWP) / CO.
*PVR = (mPAP – PAWP) / CO.
- PAWP ≤15 mm Hg
- PVR* >2 WU
- mPAP >20 mm Hg
- Normal15: 14 ± 3 mm Hg
