Overview of the 2022 ESC/ERS Treatment Guidelines
Pulmonary arterial hypertension (PAH) treatment guidelines provide a road map to managing your patients with PAH. Worldwide experts in PH review current data to inform overall care and treatment recommendations based on therapies available in Europe. These recommendations form the basis of the treatment guidelines issued by the ESC/ERS every 5 years. The most recent version of the guidelines, the 2022 ESC/ERS Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension, were released in 2022.1
Watch highlights of the 2022 ESC/ERS Treatment Guidelines
The 2022 ESC/ERS Treatment Guidelines include1:
- Updated hemodynamic definition of PAH: mPAP >20 mm Hg (at rest), PAWP ≤15mm Hg, PVR >2 WU
- Revised PAH diagnostic algorithm
- Increased importance of risk stratification to determine initial therapy and frequent re-assessment to determine treatment adjustments
- Introduced a revised methodology for baseline risk assessment that includes more hemodynamic and right heart variables
- Outlined more frequent use of echocardiography to assess therapy response and disease status
- Recommended consultation with PH Expert Centers throughout the course of disease
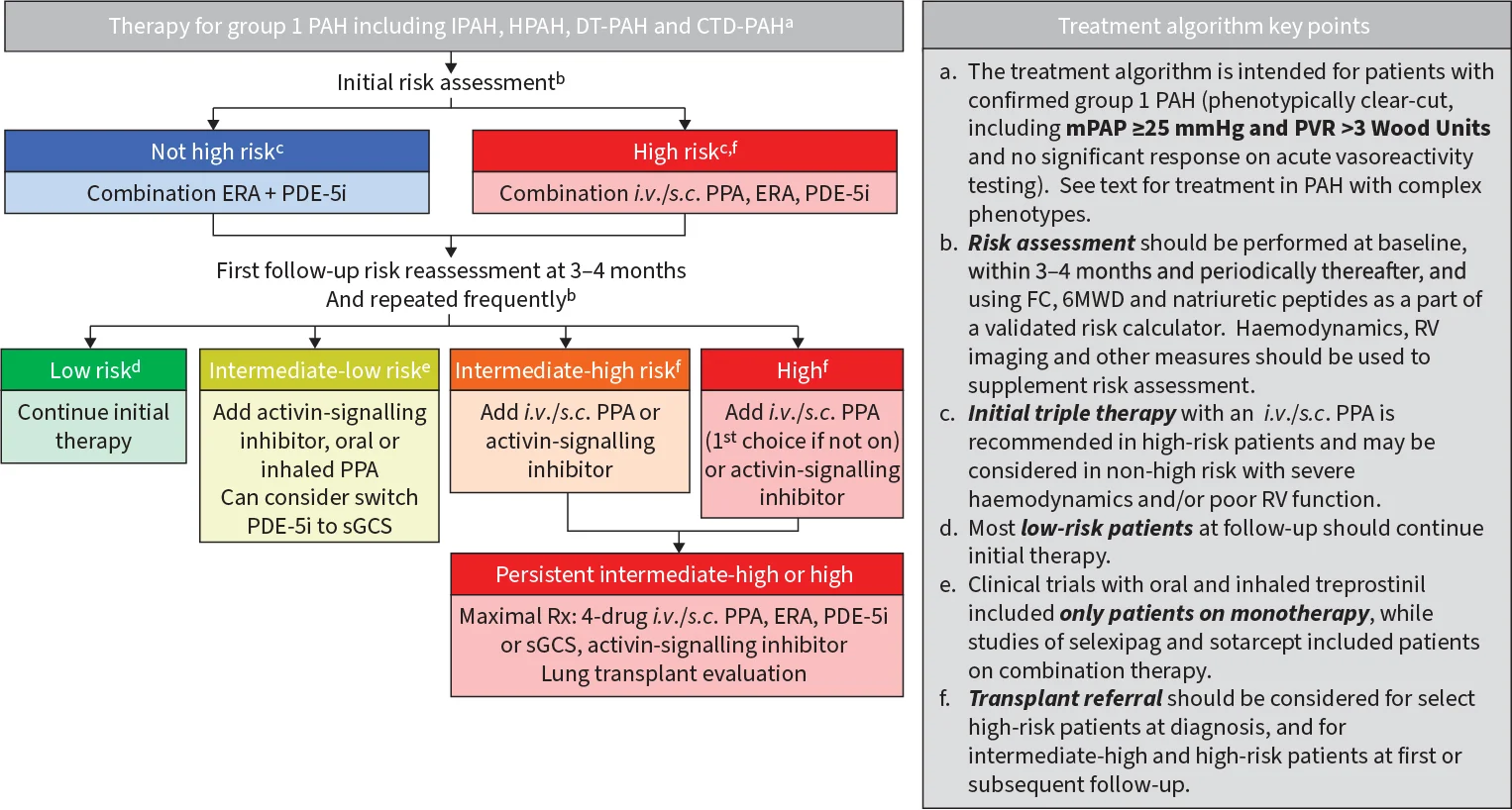
Treatment algorithms
There are many ways to care for patients with PAH, including multiple therapies that enable you to tailor treatment regimens to meet your patients’ specific needs. These 2 treatment algorithms were developed by experts to help guide decisions when setting treatment plans.1
Assessment at diagnosis
The 2022 ESC/ERS Treatment Guidelines recommend using an objective, multiparameter risk calculation upon diagnosis of PAH to establish the patient's baseline risk status. They also recommend using patient risk status to guide treatment initiation involving multiple therapies for appropriate patients.1
Click on the image to view the recommended initial treatment algorithm.

Follow-up assessments
Frequently assess progress to low risk with a 4-strata risk assessment. Prompt adjustments to the treatment plan are recommended for patients not at low risk to help improve their risk status and outcomes. Following the initial visit and treatment, guidelines recommend checking a patient’s risk status frequently, every 3-6 months at follow-up.1
Click on the image to view the recommended follow-up treatment algorithm.

Explore the Treatment Guidelines
Download 2022 ESC/ERSConsensus statements from the WSPH
In 2024, a panel of worldwide PAH experts convened for the seventh time in more than 50 years to review current considerations in PAH care.2 From this meeting, the WSPH issued a series of papers providing their perspectives for many aspects of PAH care, including diagnosis, risk assessment, treatment goals and approaches, and other aspects of patient management. These consensus documents are comprehensive reviews of large volumes of data and provide recommendations for patient care.3-17
Examine list and links to expert recommendations
Download 2024 WSPH7th WSPH treatment algorithm
One WSPH task force discussed creating an updated PAH treatment algorithm based on the ESC/ERS treatment algorithms. Because the task force reviewed newer data from the US and elsewhere, the WSPH treatment algorithm contained updated information on hemodynamics, right heart dysfunction, and treatment pathways.12
Click on the image to view the WSPH treatment algorithm.
Experts discuss the 2022 ESC/ERS Treatment Guidelines
The PAH Initiative convened a panel of US-based PAH experts to discuss the implications of the 2022 ESC/ERS Treatment Guidelines for practitioners in the US. This resulted in additions to the Advancing PAH Care video series that offer insights into patient care, treatment, and management strategies for PAH.
Each video features a conversation between 2 PAH expert clinicians describing key aspects of the latest 2022 ESC/ERS care and treatment guidelines. The PAH experts explain how these care approaches can be utilized by US practitioners to help improve patient outcomes.
With support from UT, the PAH Initiative provides nonbranded, disease education for the PAH Community. The Initiative worked with PAH experts to identify the content for this program.
Welcome. My name is Dr. Jean Elwing and I'm a professor of medicine and the Director of the Pulmonary Hypertension program at the University of Cincinnati. And I'm joined today by Dr. Scott Visovatti. Scott, welcome.
Thanks, Jean. I'm Scott Visovatti. I'm an Associate Professor of Medicine and the Director of the Pulmonary Hypertension program at the Ohio State University. I'm also a cardiologist.
So, Jean, let's give a bit of an overview on how these guidelines were developed. They were developed in Europe by a multidisciplinary group. You and I probably practice a bit differently here in the United States, as do many of the practitioners who are listening in to this video series.
Let's talk about some of those major themes that we'll hear about throughout the rest of this series.
We now approach pulmonary arterial hypertension as a hemodynamic condition and therefore it requires a hemodynamic definition. It's important to talk about how risk assessment at baseline and at follow-up is incorporated into recommendations about treatment decisions.
It's also critical to touch on the critical symbiosis between a local practitioner and a referral to a PH center and how this combination of expertise works in a patient's advantage.
So, Jean, the hemodynamic definition of pulmonary arterial hypertension has been debated for many, many years, including since the last world symposium. What are your thoughts about the implication of this new definition?
This is a very hotly debated topic. So, as we remember
we defined pulmonary arterial hypertension as a mean pulmonary pressure of 25 or greater with a wedge of 15 or less and that PVR greater than three. But we learned through big datasets that those individuals that had that mean pulmonary pressure in that what we used to call borderline range, 20-25, had increased risk of poor outcomes and mortality.
When the group assessed the data in this new ERS/ESC guidelines, they found that
even those patients that had that lower mean pulmonary pressure, that greater than 20 pressure, if they had a high resistance in their pulmonary vascular circuit – even when it was over two – they had worse outcomes. So, they proposed a new definition.
But they didn't stop there. They also looked at exercise. And we have been looking at exercise for so many years, trying to find really what we would use as a cutoff. And they proposed a mean pulmonary pressure change over cardiac output slope of greater than three millimeters of mercury as an abnormal finding.
So, where are we gonna take that? I'm not sure yet. But we will need to be able to study that group of patients further, see how they do over time, and maybe determine if they would need treatment at some point.
But currently, the only people we really recommend treatment in general to are people that meet the traditional, the older definition, because that's what we used in all of our clinical trials. You know that.
So, those other individuals with that lower mean pressure, the lower PVR, they are the people that really we want to see in expert centers. We want to evaluate. We want to see what the trajectory of their disease is and then understand when we need to offer treatment and when it's appropriate.
So, Scott, another area of the guidelines that has really evolved is risk assessment. And we had some changes in the new guidelines. What do you think about those?
Never before has risk assessment been woven throughout the entirety of guidelines. Very, very important. Important to assess risk at baseline, which we've done. Equally important to reassess patients frequently, generally every three to six months, with risk reassessment at that time as well. Our goal being to drive risk to the low risk category. And only with frequent reassessment is that possible.
Risk also helps fuel our approach to treatment, escalation of therapy based on risk. Critically important.
So, Jean, could you give us a brief overview of how risk assessment helps dictate treatment options in the new guidelines?
With our new guidelines, the 2022 ERS/ESC guidelines, we're seeing patients, evaluating, diagnosing them based on our new hemodynamic definition. And then risk assessing. We wanna know severity of illness from the get-go.
And those patients that are low or intermediate risk, we'll start them on two oral therapy. And those individuals who are on the high risk, we're going to treat them as aggressively as we possibly can with our oral therapies in addition to a parenteral prostacyclin.
But we're not gonna stop there. We're gonna reassess with the 4- strata model, as you mentioned, looking at walk distance, BNP, and functional class, and then see where they fall. Are they really getting to that low risk? And if we are, then we're happy. We're gonna hold tight.
If we're in that low intermediate, we're either gonna change medications or add medications. And if we're anything high – high intermediate or high risk, we either need to progress increasing our parenteral prostacyclin or add one.
So, really helpful in giving us a nice framework. Now, do we have to use this 4-riskstrata? Of course not. We can use REVEAL. We could use a French scoring system. But we have to do something. We are doing our patients an injustice if we don't reassess them.
Scott, another area that the guidelines stress is collaborative care in expert centers. How do you apply that to what we're doing in the US?
In Europe, by and large, it's a spoke and hub system where patients are evaluated locally but then all referred to a major center where expert opinion and can be leveraged and administered.
Things are a little bit different, as you know, in the United States, where we have very good folks who are practicing pulmonary hypertension in local centers.
There are huge benefits to having a patient evaluated at a PH center. Certainly, this takes more account how complex PAH is, not just the diagnosis, but we have more treatment options now than ever. And it's important to make sure we find the right fit for the right person. In other words, not every medication or very combination approach is right for each individual.
Jean, could you summarize some of the key takeaways of our discussion today?
So, we talked about pulmonary arterial hypertension is ever evolving.
Diagnosis and care has evolved. New medications, new risk assessment strategies. But the most important thing is that we continue to evolve and learn additional things, how to positively impact our patients.
And, really, we have to leverage, as you mentioned, the accredited expert centers and the local physicians and work together for best outcomes.
So, we've covered only a small bit of what was stressed in the guidelines, but some very important points. And we invite everyone to join for future videos about the new updates from the guidelines from 2022 ERS/ESC.
Scott, thank you so much for joining me. It was a pleasure to talk with you about the guidelines.
Thank you, Jean. I always learn something sitting with you, listening to you. Really appreciate your input.
Thank you for watching. This program is part of a series of videos about how PAH management has evolved in recent years.
Topics covered in this series include the importance of hemodynamics, the role of risk assessment, the PAH treatment algorithm, and considerations for the treatment of PAH.
For more information on PAH, please visit: ResourcesForPAH.com
Overview of the ESC/ERS 2022 Guidelines
With support from UT, the PAH Initiative provides nonbranded, disease education for the PAH Community. The Initiative worked with PAH experts to identify the content for this program.
Hi, I’m Ray Benza. I’m a professor of medicine at the Icahn School of Medicine at Mount Sinai New York City. I’m also the network director for the Pulmonary Vascular Disease Program at Mount Sinai Heart. And I have the pleasure today of being joined by my colleague and long-term friend, Dr. Vallerie McLaughlin, to discuss risk stratification in the context of a video series on the evolving management of pulmonary arterial hypertension. Val?
Ray, thanks so much. It’s a pleasure to be here with you today. I’m Vallerie McLaughlin. I’m a cardiologist and endowed professor of medicine at the University of Michigan, where I also direct the Pulmonary Hypertension Program. I’m really excited to be here today to talk about risk stratification with my dear friend, Ray.
Now, Ray and I have been doing pulmonary hypertension for a long, long time and there’s been a lot of progress in patient care. And a lot of progress in what we’ve learned about risk stratification, including so many sentinel publications that Ray has led from the REVEAL Study.
Now, when we think about risk assessment, we really need to concentrate on objective, multi-parameter risk assessments. We never rely on any one variable in assessing a patient’s risk. PAH is a complex disease; we really need a big picture of the patients.
The risk scores help us provide a consistent objective method to follow the patients over time. Really, much better than assessing one thing like functional class, or relying on gestalt. Just the eyeball test. And it helps us establish treatment goals.
We have very well-established data now that tells us, our goal should be to get a patient to low-risk status. We know that their prognosis is going to be much better if we get them there. And using risk assessment tools can help clinicians alter the treatment strategies, if a patient is not at low risk. And follow-up assessments need to be done regularly.
Every single encounter with a patient is an opportunity for risk assessment and adjustment of therapy. So Ray, why don’t we start out by talking about what risk stratification tells us about the patient prognosis and treatment goals?
Well, it can tell us quite a bit. And I would love to remind everyone that this whole evolution of risk stratification really stemmed from the work that you did such a long time ago. And published in that beautiful article in JACC, where the first risk table was published. And I always remember that table, looking at it and saying to myself well, it is better to use more than one variable at a time. Because it really paints a better picture of how a patient is gonna do with this disease.
Particularly, because it’s such a progressive disease. And I think that was one of the clues that helped me derive the original Reveal Risk Score. So, I thank you for that.
You’re most welcome.
So, risk stratification as we know, helps us predict both mortality and morbidity in patients of pulmonary arterial hypertension. And all the contemporary risk equations and calculators were derived from registry data.
From large cohorts of patients that we followed in the United States, or in Europe, including those in REVEAL in the US or COMPERA, the Swedish Registry, or the French Registry in Europe. And all of these have been used to estimate survival. And it’s important to understand that the products that came from these registries, or these risk tools that evolve from these registries, have some key differences that reflect the area of the world where they were derived from.
So with that being said, how do the patient characteristics of these registries, in your mind, apply to the patients that you see in practice?
Yeah, I think it’s a great question, right? Because we think of PAH and sometimes we think of the clean PAH that we enroll in clinical trials and that’s a very clean population. But it’s not what we see every day. And so, the registries really reflect more real-world data. The REVEAL Registry is a US registry, so it really is reflective of the patients that you and I see every day.
The French Registry, they actually are a lot tighter on their entry criteria and in many ways, it looks more like a clean-cut Group 1 PAH population. They have some heritables, they have some drug and toxin induced.
The COMPERA registry actually is older and with a lot more co-morbidities than what we see in the US. So, they’re actually three very different registries.
So, thanks for going through those individual characteristics of those registries. I think that’s important for the audience to recognize. But let’s continue.
Risk status is important in setting goals of treatment and establishing treatment and for monitoring plans. And determining when treatment adjustments may be needed. The ESC and ERS guidelines recommend a goal of low-risk status for all patients of pulmonary hypertension. And I know that I practice that, and I treat to low risk.
Patients at low risk have the highest survival rates at five years. And even those in intermediate risk, we have to remember that their survival is less than 95%. That’s really important so, just because someone is intermediate risk doesn’t mean we can leave them alone. That’s actually a very important group that we need to focus on and to drive them to low risk. Because a stable intermediate risk doesn’t mean they’re risk free. They are still at very high risk of death. So, getting those clinically stable intermediate risk to low risk is key.
And so, I wanna make sure that people understand the difference between clinical stability and low risk, it’s not the same thing. We want to treat to low risk.
It’s really essential also, I think, to avoid underestimating risk in this population. Pulmonary hypertension is a rapidly progressive, deadly disease. You don’t wanna make a mistake with that first discrimination and that first calculation of their risk. Because if you do, you won’t use the same intensity for that initial therapy as you would, and someone can get hurt by that.
We need to use these comprehensive risk assessment tools that have very good discrimination.
So Val, how would you describe how the treatment guidelines characterize baseline risk assessment?
Yeah, sure, this is really, really critical. Remember, when we’re first meeting a patient and making a diagnosis, we’re doing a very thorough evaluation. We have more data at that time than we probably have at any other time. And so, we can do a comprehensive risk assessment that includes everything we do in clinic like hall walk, labs, and such. But also echo, right heart caths, sometimes MRI. We have a lot of information. And so, going back to that risk stratification table, the low, intermediate, high.
It’s been interesting to see what’s been added in the ESC/ERS guidelines this year. So, there’s some new information about TAPSE, PAPSE, about right heart function. So, the TAPSE divided by the pulmonary systolic pressure gives us an indicator of RV-PA coupling, which we think is very, very important in pulmonary hypertension. There’s some additional MRI parameters added.
And so, really it warms my heart to see more indicators of right heart parameters in the risk stratification table. And Ray, you and I are cardiologists. We are very passionate about the right ventricle. Tell me your thoughts about these additional parameters?
Yeah, I think they’re invaluable. And do you know all the contemporary stratification schemes that we’ve developed, we always knew we were gonna have to add additional factors.
We have advanced so much in what we can do now with our imaging parameters that we get much better quantitative information from them. And I think that needs to be incorporated into our risk stratification tools. Because if you think about it, all really the variables that we have in all these scores really describe how the right ventricle is faring in the face of this very high afterload that is characteristic of this disease. So, why not have the most direct assessment of the right ventricle in imaging parameters.
Yeah, absolutely. Now, it doesn’t mean if you don’t have one parameter, that you can’t calculate a risk score. You still do it. But I do think it’s important to have all that data at baseline. And remember, low-risk status is the treatment goal, and we have to reassess risk every time we see the patient.
The intermediate-risk group is a wide range. It has a one-year mortality between 5 and 20 percent. So, that’s a really wide range. And it really emphasizes why the goal is low risk.
So Ray, you’ve really made so many important contributions to the literature with REVEAL. We’ve learned so much from the work that you’ve done. Why don’t you tell us a little bit about the REVEAL risk scoring methods and describe how the ESC/ERS updates align with the approach that you took in REVEAL.
Yeah, thank you. I think that’s a really important thing for people to understand that these algorithms are very similar. It’s the way that the multi-variables were put together where the biggest differences are.
In REVEAL, we used more of a statistical approach, where we used statistical weighting of the variables. So that, we know how one variable relates to the other variable very tightly. And that allowed us to develop algorithms with very high discrimination. Meaning that, we’re very likely to depict how a patient will live or if a patient will die, using these statistical modeling that we did. But the parameters are very similar, and many of them are in the European Risk Table.
So Ray, that’s a really great description and of course, it’s wonderful to have all that data at baseline and do the full comprehensive assessment. Now, let’s talk a little bit about how you use REVEAL 2 in follow up of patients, right? Because that’s really critical too. The goal is getting to low-risk status. So, tell me about how you incorporate that into the care of the patients?
One of the things that we were taking into consideration, when we did derivations of the REVEAL 2.0 score is, we had to take that into context of a very clinical, busy environment.
And so, we developed an abridged form of REVEAL 2.0 called REVEAL Lite. And abridged in meaning that we are utilizing only the changeable variables in this scoring system, as opposed to REVEAL 2.0 which had immutable risk factors in it like gender and age and the type of pulmonary hypertension.
But you only use the changeable risk factors. The vital signs, the renal functions, natriuretic peptide levels, the walk distance, and the functional class when you make that determination. So, REVEAL Lite 2 provides an accurate discrimination between risk with fewer variables than REVEAL 2.0 does.
And then I mentioned earlier, the 2022 guidelines present a similar model in the four-strata model. And I’d like to ask you, this model which was derived in part from REVEAL Lite. How do you think that fits in to our overview and how we approach the patient’s risk status?
So, when we think about how the ERS/ESC guidelines initially did risk, there were only three risk strata. We had variables that were low, intermediate and high risk and you calculated the score based on the variables that you had, low, intermediate, high.
So, that intermediate risk group is big, in terms of percentage. And big in terms of how we might approach treatment. So, the group from COMPERA looked at this and said, maybe there’s some way to discriminate this a little bit more. And so, they took their registry, over 1, 600 patients, and they divided them into four groups, rather than three. Low, intermediate-low, intermediate-high and high. And they used cut points derived from various registries for six-minute hall walk, functional class, and biomarkers.
So, the five-year survival between those intermediate-low and intermediate-high groups is 67% versus 47%. It’s a big difference. So, I think it’s really practical in terms of explaining things to patients, and in terms of making treatment decisions.
Now, REVEAL took a little different approach to that. Can you tell us about that?
Yeah, thanks. That’s a really key piece to really understand about the way REVEAL is supposed to be used. REVEAL is a continuous scoring system.
But using it as a continuous measure, where you have a score from 1 to 21, you can get a really nice separation of the various risk levels within that intermediate risk. It’s always been there. And it’s a good thing to recognize that you can get that level of discrimination in that intermediate group, using the continuous scoring system of REVEAL.
Let’s change gears a little bit.
So, can we talk a little bit about some of the other aspects you consider, when you decide what to do, how to manage your patients with pulmonary arterial hypertension?
Sure, I think that’s a really great direction to go in. I think we need to remind ourselves that our treatment goal is to achieve low risk for as many patients as we can do.
Because we’ve demonstrated better survival is associated with this low-risk status. And that’s my goal, that’s your goal and that’s what we should be teaching all of our colleagues who treat these patients in the community.
All risk tools have advantages and disadvantages and none of them can perfectly predict prognosis.
So, there is better need for integration of other tools into these parameters.
Particularly, imaging variables, so that we can better reflect on prognosis and make better predictions. So, these are a couple of my suggestions. So, Dr. McLaughlin, is there anything that you would like to add to this?
I think we feel both, very passionately that we are dedicated to taking care of PAH patients. But we want to work with our local docs. And it really takes a village to take care of the PAH patients. And then the other thing I wanna acknowledge is all the people that help us do this.
Yeah, those are really valuable points. So, I wanted to thank you, Dr. McLaughlin for sharing your incredible experience and providing your perspectives on how risk stratification can be useful in clinical decision making, at diagnosis, and throughout treatment.
The next video in this series, and you might wanna watch that, really builds on the story that we’ve created by focusing on right heart dysfunction, as an important indicator of disease status and patient prognosis.
In the meantime, I’d like to rehash some of the key points that we made on this talk today. And to leave our audience with some important caveats. First is that, comprehensive risk stratification is an essential part of patient management. Early and frequent risk assessment provides a timely indicator of treatment response and whether adjustments to treatment plans are really needed. As we mentioned earlier, every opportunity to risk stratify is an opportunity to help a patient get the treatment that they need.
That these treatment modifications should be based on objective risk stratification results, not just on clinical gestalt. And PH requires a proactive management scenario. It’s an entire village. So, collaborating with PH specialists and experts can really ensure that patients are optimally treated.
So, I wanna thank you again for being here with me today and it’s so great seeing you back here at the University of Michigan.
Ray, thank you so much. I always learn something every time I talk to you, and I really enjoyed our conversation today. Thank you.
Fantastic.
Thank you for watching. This program is part of a series of videos about how PAH management has evolved in recent years.
Topics covered in this series include the importance of hemodynamics, the role of risk assessment, the PAH treatment algorithm, and considerations for the treatment of PAH.
For more information on PAH, please visit: ResourcesForPAH.com.
The Role of Risk Stratification
With support from UT, the PAH Initiative provides nonbranded, disease education for the PAH Community. The Initiative worked with PAH experts to identify the content for this program.
I'm Dr. Paul Forfia, a cardiologist and professor of medicine and co-director of the Pulmonary Hypertension Right Heart Failure and CTEPH Program at Temple University Hospital in Philadelphia and I am joined today by my partner, Dr. Anjali Vaidya.
Hi, I'm Dr. Anjali Vaidya, also professor of medicine and cardiologist at Temple University Hospital in Philadelphia, co-director of the Pulmonary Hypertension Right Heart Failure and CTEPH Program.
In this program, we're going to discuss right heart parameters, echocardiography and PAH, how these findings impact care decisions and how echocardiographic findings are implemented into the updated ESC/ERS guidelines.
Dr. Vaidya, when we think about echocardiography, what are some of the echo findings that you think about when you're suspecting a diagnosis of PAH?
When I think about the views on an echo, one of the most helpful is that apical four chamber, sort of that money shot for pulmonary hypertension. And what we're looking for on this view is really evidence of the size, shape, structure, and function of the right heart parameters.
If the RV to LV ratio is enlarged, greater than one, that's very suspicious for pulmonary arterial hypertension.
Speaking of chamber size, the right atrium can also be assessed in size there which can be helpful down the line, even in our risk assessment. We're looking for the presence of a paracardial effusion in that view, which can also be a sign of very advanced disease and high-risk assessment in PAH.
And then, we're also looking for things like right ventricular hypertrophy, which is a sign of chronic afterload to the right ventricle, and then, an open RV apex, that angle of the RV apex being open rather than narrow. And that specifically is a marker of elevated pulmonary vascular resistance.
Now, other views on the echo that are also very helpful, the parasternal short axis to the mid cavity of the LV where you're looking for that septal flattening, that D-shaped septum, and that's what's traditionally described as septal flattening, reflective of RV pressure overload, but of course, what we know is it's really specific to afterload or that elevated pulmonary vascular resistance that you would see in PAH.
The other thing on echo that's really helpful on that initial diagnostic assessment is the pulse-wave Doppler in the right ventricular outflow tract, and of course, as you know, we're looking for that notching, or that reduced acceleration time, both of which are very predictive of a high PVR in PAH.
Now, all of that describes looking at the pictures directly, the images for echo, but you can also use routine echo reports to predict hemodynamics and help in the diagnosis of PAH, as well. So, there's something called VEST, the Virtual Echo Screening Tool, that we published years ago looking at routine parameters on echo and coming up with a simple score to predict if the pulmonary hypertension is due to left heart congestion, pulmonary venous hypertension where we would expect things
like an enlarged left atrium, an elevated E to E prime ratio, and numeric quantification to predict left heart congestion, and the absence of septal flattening. The flip side on a VEST score would be features that would give you a positive score, such as a normal left atrial size that the presence of septal flattening and a low E to E prime. And a positive VEST score is extremely predictive of pulmonary arterial hypertension.
So, echo can be used a lot in the initial diagnosis of PAH. In addition to echo, though, how do you use right heart catheterization in your diagnostic assessment of pulmonary arterial hypertension, but then, also, over time in your risk assessment?
Sure, so as we know, in order to make a formal diagnosis of pulmonary arterial hypertension, it is required that we obtain a full hemodynamic interrogation through invasive right heart catheterization and this allows us to measure pulmonary artery pressure, right atrial pressure, left atrial pressure, cardiac output, and then, derive pulmonary and systemic vascular resistance.
So, when we think about how we use right heart catheterization at the baseline diagnosis, the things that I'm most interested in, how high is the PVR and how affected is the cardiac index, and how elevated is the right atrial pressure?
It's not surprising to know that on serial assessment PVR, cardiac index, and right atrial pressure are also very important to follow in patients serially on therapy. In fact, one of the most important parameters to see on follow-up hemodynamic assessment of a patient is what their cardiac index is on PAH medical therapy. This is far more prognosticating than even their baseline cardiac index is.
Dr. Vaidya, how do you use echocardiography to serially assess patients once a diagnosis of PAH has been made?
So, on the echo, we're looking at RV function. TAPSE, for example. We're looking at more extreme metrics that represent really severely decompensated right heart, so when the right heart is chronically congested and impaired in function and you have impairment of venous and lymphatic drainage via the coronary sinus, you can develop that transudative pericardial effusion.
Right atrial size actually has been shown to be predictive of risk in pulmonary arterial hypertension. To some extent, we're looking for reversal of some of those other diagnostic features, like improvement of that septal flattening, for example, and the overall improvement in RV morphology. But importantly, not just the assessment of the right heart on echo, it’s worth talking about the frequency of use of echo in the risk assessment in PAH.
So, we've learned over the years, and the guidelines, the ESC/ERS guidelines, also emphasize this; that echo should be used more frequently than it previously had thought to be. And so, at least every three to six months of using echo in risk assessment for PAH. And we've learned that frequent monitoring with echo actually improves our ability to accurately risk assess patients
Now, in addition to the echo and the hemodynamics, in terms of the risk assessment in PAH, how do you incorporate both of those things in conjunction with some of the other important clinical parameters such as six-minute walk distance, functional class, or NT-pro BNP?
In order to best answer that question, I'd like to go back to thinking about the hierarchy of living systems and I think about organs, organ systems, and organisms. And so, the organ that's affected in PAH at the outset of disease is the lung and the lung circulation. And as that lung circulation is diseased and the pulmonary vascular resistance goes up, that affects the right side of the heart. That's your organ system. It's the lung and the heart.
And so, I think of that as the leading indicator of the disease, and then, I think about things that stem from that and happen later.
What can happen next? Your BNP is going up. What can happen thereafter are things that are a bit more pathophysiologically removed from those kind of core pathophysiologic changes, like a person is saying, "I'm more short of breath when I'm walking". Their functional class will rise. Their six-minute walk distance may go down. Ultimately, if those abnormalities persist, a patient may actually transition into having clinical right heart failure. You'll start to see fluid retention and even the patient may become hospitalized from de-compensated right heart failure.
And so, I like to think of the cardiac imaging findings as a leading indicator, and then, some of those more further removed parameters as lagging indicators. As you know, one of the key goals in the management of PAH is to actually get the right side of the heart to as close to normal in size and function as possible.
So, that's a really nice summary and actually ties into what we've often said about take a look at the heart to see what's happening in the lungs, which of course is then a predictor for what would happen to the patient entire. So, we've talked about a lot of components today of the right heart, and just to summarize, initially really looking at the echocardiogram to use parameters to help make the diagnosis of pulmonary arterial hypertension.
We've talked about the hemodynamics that are really important to support that diagnosis, and then, shifting gears into risk assessment, we've taken a bit of a deeper dive into looking at how the echocardiogram can represent markers of risk from the right heart and also how you use those complimentary hemodynamic parameters to help predict risk in PAH over time.
And so, it's important to partner with our sonographers and our technologists to ensure that they’re able to obtain high-quality comprehensive echocardiography to make these assessments that we discussed, and it's important for the physicians to know that if we don't have access to that kind of echocardiography expertise, then, per the guidelines, it really would be very important to refer patients to accredited centers of pulmonary hypertension expertise who can then have access to that quality of echo.
And so, we've had a wonderful conversation talking about pulmonary hypertension and the right side of the heart and how it's been incorporated into the most recent ESC/ERS guidelines, and we're really delighted to partner with our colleagues who are continuing that conversation of how to use the ESC/ERS 2022 guidelines in the clinical care of pulmonary arterial hypertension.
Thank you for watching. This program is part of a series of videos about how PAH management has evolved in recent years.
Topics covered in this series include the importance of hemodynamics, the role of risk assessment, the PAH treatment algorithm, and considerations for the treatment of PAH.
For more information on PAH, please visit: ResourcesForPAH.com
Understanding the Right Heart Beyond Pressure
With support from UT, the PAHI provides non-branded, disease education for the PAH Community. The Initiative worked with PAH experts to identify the content for this program.
I’m Franck Rahaghi, chair of pulmonary and critical care at the Cleveland Clinic in Florida, and the director of pulmonary hypertension program. I’m joined here by my colleague, Dr. Mandras.
I’m Dr. Stacy Mandras, the medical director of the pulmonary hypertension program and a transplant cardiologist at Advent Health in Orlando.
In today’s discussion, we will review the updated treatment algorithm that was published in the ESC/ERS treatment guidelines released in 2022.
Highlights from the guidelines include clarified treatment goals, strength in need for proactive, risk-based approach to treatment plans, the recommendation to use baseline and frequent follow-up risk assessments, an expanded risk assessment approach to include right heart parameters, and lastly, added guidance for patients with cardiopulmonary comorbidities.
So, Franck, with those key points in mind, let’s talk broadly about the PAH treatment approach before we explore specifics around the treatment algorithm. What are your thoughts?
Yeah, so, I think one of the hallmarks of this version of the guidelines is actually frequent risk assessment. In the past, we used to focus on patients’ functional class and symptoms, and really, truly, risk assessment is a much better way to determine where the patient is in their evolution and what do they need next?
And again, another approach that we’re going to take is not just be happy with necessarily the lower risk, but actually look for actual clinical improvement and having clinical improvement in mind.
So, let’s get into some specifics, Stacy. What do the guidelines recommend for initial management?
So, baseline risk assessment is recommended at diagnosis, and options include either the ESC/ERS 3-strata method, or, like we use in my practice, the REVEAL 2.0, and these are validated risk assessment tools that
Give us a much more comprehensive idea of whether the patient falls into a low, intermediate risk, or high risk, and treatment options depend on where they fall.
Most patients, it’s recommended, start on combination therapy up front. We learned from the AMBITION trial that patients who are started on combination ERA PDE5 do better than patients who are started on monotherapy with either one alone.
The guidelines recommend as initial therapy that patients who are low or intermediate risk are started on this combination of the ERA and PDE5. That said, patients who have severe hemodynamic impairment, either by echo or hemodynamics with the right heart cath invasive data, despite being intermediate risk, these patients should be considered for parenteral prostacyclin as part of their upfront combination therapy.
For high-risk patients, these patients truly should be offered parenteral prostacyclin upfront, either IV or subq. It’s a conversation that you have to have with your patient, as there may be reasons why some patients are better candidates for one or the other.
And then lastly, patients who have certain cardiopulmonary comorbidities, like hypertension, obesity, these patients may also be considered for monotherapy upfront, but these are patients that you need to monitor closely.
So, with this overview of initial therapy recommendations, let me ask, Franck. In what ways does your follow-up management approach either align or differ with the guidelines?
So, actually, to a great degree, they do align. So, it’s really important to have treatment goals, which we already had discussed involve getting the patient to low-risk status within a year or as soon as possible, frequent risk assessment, usually every three months seeing the patients, and it’s really important to be aggressive.
It’s kind of akin to the golden hour of sepsis, where you have a limited time to get the patient better. Studies have shown that if you don’t get them to low-risk status within a year, they will have poor outcomes. And that’s why we sort of use the risk assessment frequently, and in the follow-up, we now use the four strata risk assessment.
In the past, and using, for instance, REVEAL 2.0, we sort of, in our minds, used to divide them in the sort of the low intermediate and high intermediate, and here, now, the criteria have been formalized for that, because we know that the low intermediate, as you explained, and the high intermediate have a differing way of following the patients.
Now, in addition, the guidelines have suggested, and we believed in it, that you have to also consider right heart parameters.
As an example, I have a patient, I had a patient that was low risk, technically, but had a really dilated right ventricle, and this young woman with two kids, I figured that if something happens to her, she has no reserves. So, even though she was at low risk, technically, I escalated her care so that the right ventricle would shrink, and indeed, that’s what happened. So, an example of how to incorporate the right heart parameters on top of the guidelines.
And then, again, treatment follow up is key, once you start something, to go back and check and see where the patient is clinically and where their risk are, so that you could escalate or continue the care.
The next question is, how do you determine when and if to make changes in the treatment plan, Stacy?
So, as you said, everything is based on trying to achieve a low-risk strata. So, if I see patients on follow-up, even on the very first follow-up, if I don’t see them improving from intermediate or high risk coming down toward low risk or achieving low risk, then we have to escalate therapy.
If at baseline they’re low risk and they maintain low risk at follow-up, we maintain their current regimen. If they were at increased risk, whether it’s intermediate or high risk, and they achieve low risk at follow-up, they stay on the therapy that they’re on.
If they’re intermediate low risk, I would argue that is not good enough. I think most of us would argue, that is not good enough. Every patient should, if possible, achieve low risk status, and so if they come on follow up and they’re intermediate low risk, then those patients deserve some type of treatment escalation,
either transitioning from the PDE5 to the guanylate cyclase stimulator or addition of some form of prostacyclin therapy, whether it’s oral, IV, subq, or in the US, inhaled, which is not available in Europe, but for us offers a nice additional tool in our arsenal, as it tends to be fairly well tolerated and demonstrates improvement in six-minute walk and functional capacity.
For patients who are at intermediate-high risk, those are patients, again, who should be escalated, and in that stance, I would say those are patients who should be offered parenteral prostacyclin. Again, they have a choice between IV or subq, and that’s a conversation that has to happen between the provider and the patient.
Sometimes there are other things that go into play, things like support, distance from the treatment center, etc. So, again, this is very much individualized therapy, and that includes, for patients who have the cardiopulmonary comorbidities that we discussed earlier, these patients need to be followed very closely, frequent follow up is important, patients are seen sometimes every three months, our sicker patients may be followed every one to two months.
So, we’ve gone through a lot of information here, Franck. Thank you so much for all of your insight. Would you please summarize some of the key points that we’ve covered?
Well, Stacy, thank you for your brilliant comments and your perspective. So, basically, if I want to summarize it, I would say that pulmonary arterial hypertension management requires proactive and routine monitoring and risk assessment and goal-oriented therapy based on the risk, and with the objective of getting the patient to low risk within the first year.
Thank you for joining us today for this discussion. The discussion on the treatment algorithm is only part of a series of videos that we encourage you to check out, so, with that
Goodbye
Thank you for watching. This program is part of a series of videos about how PAH management has evolved in recent years.
Topics covered in this series include the importance of hemodynamics, the role of risk assessment, the PAH treatment algorithm, and considerations for the treatment of PAH.
For more information on PAH, please visit: ResourcesForPAH.com
The 2022 Treatment Algorithm
With support from UT, the PAH Initiative provides non-branded, disease education for the PAH Community. The Initiative worked with PAH experts to identify the content for this program.
Hello and welcome. I’m Dan Lachant. I’m a pulmonologist and Assistant Professor at the University of Rochester Medical Center. I have both a clinical and research focus in pulmonary hypertension and I’m joined by my colleague, Dr. Sophia Airhart, to discuss real-world approaches for managing patients with pulmonary arterial hypertension.
Thank you. Dr. Lachant. I’m Sophia Airhart, I’m Medical Director of Heart Failure and Pulmonary Hypertension at St. Alphonse Regional Medical Center and Adjunct Assistant Professor at University of Utah, who we collaborate closely with. I’ve been an advanced heart failure cardiologist for five years and have a strong passion for treating and recognizing pulmonary arterial hypertension.
Today, Dr. Lachant and I will discuss how updates in the 2022 ESC/ERS treatment algorithm can be applied to clinical practice, and the importance of individualizing treatment plans. As you know, these patients are complex and they require a team approach for best outcomes. And that’s why we’re here, as a cardiologist and pulmonologist, discussing PH and daily clinical practice.
The guidelines focus initially on early identification of pulmonary hypertension in the community, as well as really triaging these patients who are high risk to a center of excellence.
With regard to initial drug therapy, three strata, multi-parametric model is used that estimates prognosis in one year mortality and guides treatment with the goal of achieving a low-risk status within the first year of therapy.
Early close follow-up is also recommended every three to six months, and when a shorter four strata model is used, it really focuses on functional class, six-minute walk distance, NT-proBNP. As we know, it’s not black and white.
Dr. Lachant, what are some of the key factors you consider when managing these patients?
Those are all great points that you just highlighted, Dr. Airhart.
The good news is that with new treatment strategies and medications, the outcomes have improved, and I think a lot of that’s due to frequent follow-up that you described.
Another important point to consider when treating patients with pulmonary arterial hypertension is the comorbidities associated with it and that’s where being at an expert center
really helps patients. So, whether somebody has scleroderma, cirrhosis, GI bleeding – we have specialists who are well aware of pulmonary arterial hypertension, as well as the medication side effects.
And also developing strong support systems is extremely important. We provide patients with an emergency number so they can contact us 24/7 if they have an emergency.
And finally, the biggest thing that helps these patients is just joining the Pulmonary Arterial Hypertension Association support group system. Networking with patients and families who have been through this journey is extremely valuable and can really help provide reassurance for these patients.
These are just some of the factors I think about when managing patients with PAH. Dr. Airhart, is there anything else you would like to add?
You bring up a lot of really important points and I would like to reiterate those as well, but I start with generic lifestyle recommendations as well as the importance of exercise.
So, with regard to lifestyle recommendations, I recommend limiting fluid intake to less than two liters a day and salt to less than two grams a day, but clearly it’s going to be patient dependent. I think exercise training is really important. It helps people sleep better, it decreases dyspnea, and it improves their exercise tolerance.
And are these patients able to maintain medications schedules? You had mentioned is it more convenient for them to be on BID therapy, can they handle TID therapy or is continuous therapy more conducive to their life? And so, asking all those questions to really find out who they are and how they can best support them is important.
Oftentimes, after diagnoses, these patients go online and it can be very overwhelming and they come back to your clinic the next day and they ask, “Am I gonna live? How long am I gonna live?” And I think that that is a doorway to have the conversation of risk stratification in pulmonary hypertension and how that informs treatment and why we do what we do in terms of lab monitoring and frequent six-minute walk tests so they can be a partner in their care.
We talk about escalating to parenteral therapy, I usually integrate conversations about, you know, being considered for lung transplant because I don’t want that conversation to take patients by surprise and oftentimes, they need to prepare.
So, there are a lot of nuances in PH care. Dr. Lachant, as a PH expert, what is your perspective on the role of PH centers and managing these patients?
That’s another great point you brought up about lung transplantation that ties in nicely about PH centers and experts who treat this.
What we wanna do is develop a co-management strategy.
The other thing is we also don’t want to take ownership of their patients. We like a collaborative approach, especially in patients where it’s difficult for them to travel. We like having an option locally for them to be able to still see another provider, have frequent check-ins, stagger visits.
The Pulmonary Hypertension Association makes it easy for patients to find centers across the country so if they want they can reach out. And given where we are with the advances of telemedicine, I think all patients should have at least one interaction with a pulmonary hypertension center and from there, they can decide what’s important to them, what the center thinks, what their local physician thinks in terms of who should take ownership of some of their more advanced therapies – do they need advanced therapies? But that first, initial interaction is extremely important for all patients.
One important factor in patient care is how to best manage concurrent cardiopulmonary comorbidities. Dr. Airhart, can you talk about how the guidelines recommend managing patients with these comorbidities and how these recommendations align with your current approach?
Yeah, really great question. So, when I have a patient in front of me, it’s rare that I have a patient just with PAH. Usually they have other chronic medical conditions. And so, the first question I ask myself is, is their PH due to their other medical conditions or is this PAH with comorbidities?
Well, the guidelines recommend more cautious monotherapy in patients who have cardiopulmonary comorbidities as well as more close monitoring, particularly because we know these patients with comorbidities have poorer response to PAH medications and a greater likelihood of discontinuing medications due to side effects, as well as a lower chance of reaching a low-risk status and a higher mortality risk.
Because these patients are at higher risk of side effects, we discuss side effect management proactively as we do in the PAH population and I know you do in your population, so really they can be more likely to tolerate therapy and therapy escalation because their other big risk is that these patients be undertreated.
We know that PAH is a progressive incurable disease, and we don’t wanna undertreat this higher risk population, so that’s why frequent follow-up, as well as aggressive side effect management is essential.
That’s my approach as a cardiologist, but Dr. Lachant, I’d love to hear your thoughts from a pulmonology perspective on this complex patient population.
From a pulmonary perspective or a pulmonologist perspective, the two tests I really like to look at are pulmonary function tests and CT imaging. Most patients have had these checked at some point and really what I’m looking for is do they have any airways disease.
So, depending on what those two tests show, we kind of decide with the patient collaboration of is this somebody who I’m concerned medications will disrupt their VQ matching and make their oxygenation worse? And if that’s the case and they wanna feel better, we typically admit these people to the hospital for 24-48 hours, make sure their oxygenation doesn’t get worse, then we send them home and follow them up generally in three to four weeks.
And some of our other patients where structural lung disease is less of a concern, we follow a general strategy that you described where we contact them, they keep in contact with a specialty pharmacy, they send us updates, and we generally see them within three months to make sure we’re headed towards that low-risk status.
Thank you Dr. Lachant for sharing your experience and insights on the treatment guidelines and how we really need to layer in individualized care plans. We covered a really wide range of topics that require specialized approach. What are your key takeaways from our discussion today?
Thank you, Dr. Airhart. I learned a lot from you especially how you view things from a cardiology perspective and just hearing your experience was very eye-opening and enlightening.
Guidelines can help guide treatment choices, but selecting the final treatment should be based on the individual patient situation and needs and not just following an algorithm.
The most important thing I took away was frequent follow-up is the biggest thing, especially for starting monotherapy. We wanna make sure that patients are actually improving and we’re not just settling for status quo. And co-managing patients with PH centers has many benefits and like I said before, I think all patients should have at least one evaluation with a PH center to make sure everything is the way it should be.
Yeah, I think those are great take-home points. Another thing I would add is that early recognition is really important and it’s important to collaborate with everyone out there to recognize this patient population because they’re not all in highly dense areas and the earlier we recognize pulmonary hypertension, the earlier we can treat pulmonary hypertension and the better patients do. So, thank you everyone for joining us today. It’s been a great conversation. Please check out the other videos online as well in the series.
Thank you for watching. This program is part of a series of videos about how PAH management has evolved in recent years.
Topics covered in this series include the importance of hemodynamics, the role of risk assessment, the PAH treatment algorithm, and considerations for the treatment of PAH.
For more information on PAH, please visit: ResourcesForPAH.com.
Considerations for Individualized Care
This video focuses on how updates in the 2022 ESC/ERS Treatment Guidelines can be applied to clinical practice when considering the importance of individualizing treatment plans and seeking consults with PH Expert Centers
Speakers:Dr. Sophia Airhart, Medical Director of Heart Failure and Pulmonary Hypertension, St. Alphonse Regional Medical Center; Adjunct Assistant Professor, University of Utah
Dr. Dan Lachant, Assistant Professor, University of Rochester Medical Center