Right heart changes in PAH
Although pulmonary arterial hypertension (PAH) is a lung disease, the tight coupling between the pulmonary arteries and the right heart means that PAH-associated vascular remodeling can lead to right-sided heart failure—the most common cause of death in patients with PAH.1,2
Near-normalization of right heart
Right heart health is critically important to evaluate in patients with PAH, since the size, shape, and function of the right heart are key signals of PAH disease status.3-11 One important treatment objective is to improve right heart function.12 Near-normalization of the right heart can reflect both anatomical and functional improvements of the heart, including, for instance, normalizing RVSP.3,10
Why is near-normalization important?
Quick Clips!
Watch as Dr. Anjali Vaidya and Dr. John Ryan describe the importance of near-normalization of the right heart as a treatment goal in PAH.
View the program: The Echo in PAH: Pathophysiology of the Right Heart and Treatment Goals (30 min)
[Video title: The Echo in PAH: Near-Normalization Improves Prognosis]
[On-screen text: John Ryan, MD, MB, BCH, BAO; Anjali Vaidya, MD, FACC, FASE, FACP; Excerpted from The Echo in PAH: State of the Art in Right Heart Monitoring]
[On-screen text: Anjali Vaidya, MD, FACC, FASE, FACP, Professor, Medicine, Lewis Katz School of Medicine at Temple University; Co-Director, Pulmonary Hypertension, Right Heart Failure & CTEPH Program, Temple University Hospital, Philadelphia, Pennsylvania]
Dr. Anjali Vaidya: We want to frequently monitor this and supplement it with our kind of integrated Echo Doppler assessment to help inform our treatment decisions.
It might guide us to be more proactive and progressive in our treatment escalation, than if we solely relied on Functional Class and 6-minute walk. We know that these changes to the right heart can often occur before the subjective changes, or the functional capacity may definitively change, and we certainly see that time and time again in our clinical practice. And it's really important to note that while patient symptoms are so important for them and for us, if we wait for them to worsen before we adjust their treatment regimen, we may miss an opportunity to improve their functional impairment.
[On-screen text: Excerpted from The Echo in PAH: State of the Art in Right Heart Monitoring; View the entire program at www.RightHeartInPAH.com]
[On-screen text: PAH Initiative; Sponsored by United Therapeutics; PAHinitiative.com/hcp; © 2023 United Therapeutics Corporation. All rights reserved. US-DS-1107]
Right heart changes indicate disease status
Achieving near-normalization of the right heart is a critical consideration in improving patient outcomes.3,8-10 Echo offers a noninvasive way to assess the structure of and hemodynamic burden on the right heart at diagnosis and throughout a patient’s disease progression.7,13 Echos may also help identify early signs of right heart strain before outward clinical signs are seen.7
Right heart changes can occur quickly4
Because PAH is a progressive disease, frequent follow-up assessment of the right heart is required.13 Although clinical parameters such as 6MWD and FC are commonly used to monitor patients with PAH, they are lagging indicators of disease progression, occurring after right heart changes occur.6,7
Detrimental changes in the right heart can happen in as few as 12 weeks.4 Monitoring the right heart regularly throughout treatment can reveal how well the treatment plan is working or whether therapeutic modifications and treatment escalation may be needed.3,6-8

Changes in the right heart occur before clinical changes are evident.5,6
Disease progression over time:
- Changes in the right heart
- Change in NT-proBNP
- Change in 6MWD
- Change in weight
- Change in FC
- Hospitalization

"I like thinking about the hierarchy of living systems … about organs, organ systems, and organisms. The organ that's affected in PAH at the outset of disease is the lung and the lung circulation. As … lung circulation is diseased and the pulmonary vascular resistance goes up, that affects the right side of the heart. That's your organ system: it's the lung and the heart. I think of that as the leading indicator of the disease, and then, I think about things that stem from that and happen later."
— Paul Forfia, MD, Professor of Medicine, Co-Director, Pulmonary Hypertension/Right Heart Failure and CTEPH Program, Temple University Hospital, Philadelphia, PA
Why assess the right heart?
Assessing the right heart is a critical consideration when evaluating PAH disease status. Hemodynamic measurements are integrated into risk assessment tools, giving added importance to the resulting risk score.3
A key treatment goal is to help your patients achieve and maintain near-normalization of the right heart.3 Frequent right heart Echos, coupled with risk assessment, form a strong foundation for understanding a patient’s disease status.3,12 Knowing the health of a patient’s right heart informs timely treatment decisions that can help delay functional impairment and improve patient outcomes.3,6-8
Right Heart Infographic
Use this infographic to review critical right heart assessments for PAH care.
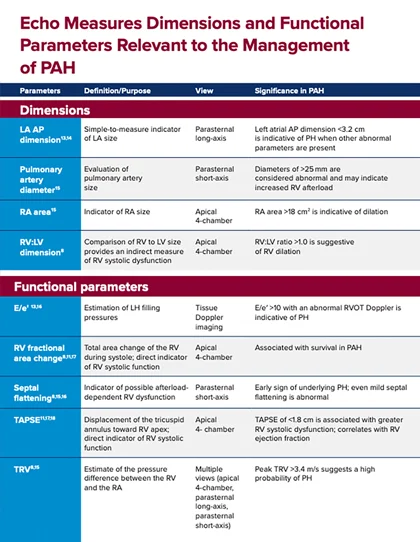
Comprehensive right heart Echo
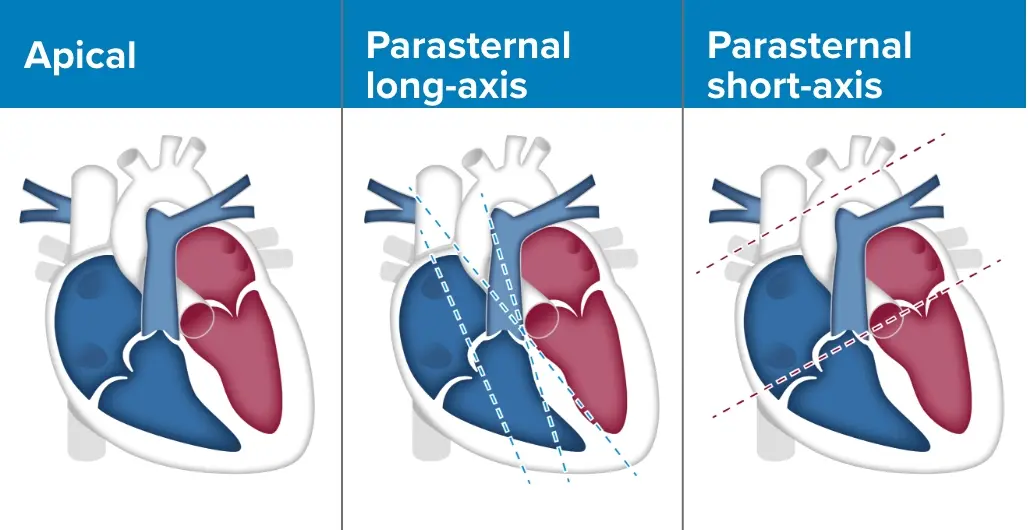
An Echo is a non-invasive, multiparameter assessment that can provide anatomical and functional markers for right heart evaluation.3,12,14
Echos should include the following parameters3,14:
- Measurements of RV size and function
- Measurements of RA size
- Relative proportions of the RV to the LV
- Estimating the RVSP
-
Estimate other functional parameters such as:
- E:e′
- RV fractional area change
- Septal flattening
- TAPSE
- TRV
RVSP approximates PASP
RVSP is a stand-in for PASP, which must be measured using a right heart cath. RVSP can be estimated by collecting tricuspid regurgitant jet velocity during an Echo.14 It should be noted that normal RVSP varies by age.14,15
Patients who have a non-normal TR jet velocity or non-normal estimated RVSP, in addition to other Echo signs of right heart strain, should be considered for further PAH screenings.3,14,16
Patient age (years)
Normal RVSP (mean)15
<50
27.3 ± 5.7 mm Hg
50-75
30.2 ± 7.6 mm Hg
>75
34.8 ± 8.7 mm Hg
The Echo doesn’t lie
Quick Clips!
Watch as Dr. Anjali Vaidya explains the role of Echo in detecting changes in right heart function.
View the program: The Echo in PAH: Right Heart Imaging in Clinical Practice (17 min)
[Video title: The Echo in PAH: “The Echo Doesn’t Lie”]
[On-screen text: John Ryan, MD, MB, BCH, BAO; Anjali Vaidya, MD, FACC, FASE, FACP; Excerpt from The Echo in PAH: State of the Art in Right Heart Monitoring]
[On-screen text: Anjali Vaidya, MD, FACC, FASE, FACP, Professor, Medicine, Lewis Katz School of Medicine at Temple University; Co-Director, Pulmonary Hypertension, Right Heart Failure & CTEPH Program, Temple University Hospital, Philadelphia, Pennsylvania]
Dr. Anjali Vaidya: There is so much variability and error in the RVSP estimation for a variety of Echo Doppler technique issues, and this has been shown time and time again, particularly some data that show up to 50% of patients will have a 10 millimeter of mercury error in the Echo Doppler estimation of pressure relative to the directly measured hemodynamics. So, the bottom line is the pressure is never the answer. It's never the answer in the diagnosis. It's never the answer in the risk assessment, even less so. It's meant to raise awareness to look closer. And once you have a suspicion of it, we have to look at all of the right heart parameters, right ventricular size, structure, function, tricuspid regurgitation, right atrial size and shape, IVC collapse, and all of those things. And so, if we do our Echos more frequently, then our clinical gestalt tends to be more in line with a formal validated objective risk assessment. And I think that point is really key. So, I always tell my fellows and my residents, "The Echo doesn't lie", whereas you just nicely presented a case where 6-minute walk and Functional Class could represent such a wide range of actual cardiac performance. So it's a long-winded way of saying more frequent is better. Any sign of a clinical change in a relatively urgent Echo, if I'm escalating therapy, or if I've recently changed their therapy, then I'm not waiting more than 3 months for my next echocardiogram.
[On-screen text: Excerpt from The Echo in PAH: State of the Art in Right Heart Monitoring; View the entire program at www.RightHeartInPAH.com]
[On-screen text: PAH Initiative; Sponsored by United Therapeutics; PAHinitiative.com/hcp; © 2023 United Therapeutics Corporation. All rights reserved. US-DS-1109]
Routine Echos catch PAH progression
Right heart Echo measurements provide insight into disease progression before clinical symptoms worsen.8 In addition, Echos can further stratify patients to give important prognostic information and determine an appropriate treatment plan, particularly for those in the intermediate-risk group (eg, those with mild or moderate PAH).11
Echos as often as every 3 to 6 months in patients with PAH3
The 2022 ESC/ERS Treatment Guidelines recommend frequent right heart Echos every 3 to 6 months to monitor disease status in PAH. Echos are indicated after changes in therapy and in the case of clinical worsening and may be considered in patients who are stable.3
Routine Echos detect changes
Quick Clips!
Watch as Dr. Anjali Vaidya and Dr. John Ryan discusses how frequent Echo assessment can lead to earlier detection of changes due to PAH.
View the full program: The Echo in PAH: State of the Art in Right Heart Monitoring (47 min)
[Video title: The Echo in PAH: Routine Echos Detect Changes]
[On-screen text: John Ryan, MD, MB, BCH, BAO; Anjali Vaidya, MD, FACC, FASE, FACP; Excerpt from The Echo in PAH: State of the Art in Right Heart Monitoring]
[On-screen text: John Ryan, MD, MB, BCH, BAO, Associate Professor, Division of Cardiovascular Medicine, University of Utah; Director, Pulmonary Hypertension Center, University of Utah, Salt Lake City, Utah]
Dr. John Ryan: The changes in the right heart are the first things that will occur, and we don't necessarily have good ways of evaluating that, other than echocardiogram. Even these changes in the right heart will precede changes in N-terminal proBNP. A lot of us depend on N-terminal proBNP in clinic, following patients longitudinally. Then you'll get a change in 6-minute walk, then you'll get a change in weight, then you'll get a change in Functional Class, and then you'll get hospitalization.
So, we don't want to progress to change in Functional Class or change in hospitalization. We want to capture this early. So, performing a routine Echo may help catch patients whose pulmonary arterial hypertension is progressing before the symptoms are evident.
[On-screen text: Excerpt from The Echo in PAH: State of the Art in Right Heart Monitoring; View the entire program at www.RightHeartInPAH.com]
[On-screen text: PAH Initiative; Sponsored by United Therapeutics; PAHinitiative.com/hcp; © 2023 United Therapeutics Corporation. All rights reserved. US-DS-1105]

“[Echo] monitoring is really critical [in PAH], and it should be done with high frequency to identify early recognition of a patient's clinical status that's declining.”
— Anjali Vaidya, MD, FACC, FASE, FACP, Professor of Medicine, Co-Director, Pulmonary Hypertension, Right Heart Failure, and CTEPH Program Director, PH Fellowship, Lewis Katz School of Medicine, Temple University, Philadelphia, PA